What is a herniated disc in the lumbar spine (LS)?
A herniated disc in the lumbar spine (LS) is a rupture of a part of the gelatinous core of the intervertebral disc through its fibrous ring. Medically, a herniated disc in the lumbar spine is also called a lumbar disc herniation or lumbar disc hernia.
To explain such a lumbar spine herniation, it is necessary to understand the function and structure of the intervertebral discs: The 23 intervertebral discs in the human body act as a buffer between the vertebrae. Each intervertebral disc is equipped with a gelatinous core (nucleus pulposus), which is encased in a hard, firm fibrous ring (annulus fibrosus). With their lamellae, the fibrous ring is intended to stabilize the intervertebral disc in their position. In the event of permanent incorrect or excessive loading and age-related wear, the elasticity is reduced and small cracks appear in the outer fibrous ring. This can cause part of the gelatinous core to escape from the ring, enter the spinal canal and press on the spinal cord with its spinal nerves. When this happens, we call it a herniated disc, which is usually very painful. The pain can radiate into the arms and legs of the affected person, tingling, numbness and paralysis can be added.

Why is the herniated disc in the lumbar spine the most common?
In fact, the herniated disc in the lumbar spine is the one that occurs most often. Nine out of ten disc patients are affected. The reason for the high percentage of lumbar disc herniations: The total weight of the spine rests most heavily on the lower intervertebral discs with their five vertebral bodies of the lumbar spine. On the one hand, nature has equipped them to be particularly strong; on the other hand, they are most frequently affected by wear and tear. Damage to the cervical spine is less frequently encountered, and even less rarely to the thoracic spine. A herniated disc alone is diagnosed 800,000 times a year. Patients between the ages of 45 and 55 are the most likely to receive this diagnosis.
Structure of the lumbar spine (LS)
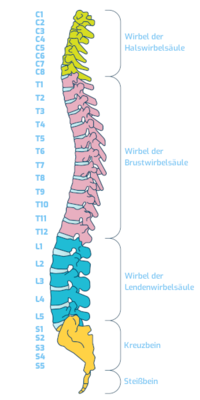
The area of the spine between the thoracic spine and the sacrum is called the lumbar spine (LS). It consists of five vertebrae and their joints, as well as the intervertebral discs located between the lumbar vertebrae.
When doctors write a prescription or formulate a discharge report, for example, they count from top to bottom, meaning L1 is at the top, followed by L2, L3, L4 and L5. The five vertebrae are in turn made up of five bony parts. These are a vertebral body, a spinous process, two transverse processes and a vertebral arch. The lumbar spine, like the cervical spine, has a physiological forward curvature (lordosis). An excessively pronounced forward curvature of the spine in the lumbar region results in a hollow back.
The sacrum and tailbone are located at the end of the lumbar spine. Everyone who has ever landed with full force on their backside knows how painful these parts of the body can be.
What are the causes of a herniated disc in the lumbar spine?
There is no one cause for a lumbar disc herniation. Rather, there are multiple causes that can lead to a lumbar disc herniation.
The most common causes of lumbar disc herniation:
- Heavy, abrupt lifting or incorrect twisting.
- A wear and tear (degeneration) of the connective tissue ring of the intervertebral disc due to age and stress.
- Overweight, lack of exercise, constant sitting, specific occupational stresses to which, for example, professional drivers are exposed.
- Jerky movements as well as sports (horseback riding, mountain biking), during which the spine is shaken or twisted in itself (tennis, squash).
- Genetically determined, i.e. predisposition, family history. Anyone who knows of such cases in the family should live a particularly back-friendly life and pay attention to a healthy posture.
- Accidents
- Smoking
- Weak or weakened muscle condition, i.e. untrained back muscles
- Rheumatic inflammatory diseases, congenital malformations, infections or osteoporosis (bone loss)
- During pregnancy due to a hormonal weakness of the connective tissue.
- A change in the spine, for example triggered by vertebral fractures, inflammatory diseases or even tumors, can be a trigger for a herniated lumbar spine disc.
Looking at this list, it immediately becomes clear why lumbar herniation cannot be attributed to a single cause. Experience shows that many factors come together to form the cause.
What symptoms indicate a herniated disc in the lumbar spine?
The symptoms of lumbar spine disc herniation are similar to the causes: There is not one symptom that indicates a herniated lumbar spine disc, usually a number of symptoms. Generally, you should keep in mind: Often, a lumbar disc herniation announces itself over several days with radiating back pain. If the pain extends into the legs and does not stop after five days at the latest, you should go to a specialist and be examined.
The most common symptoms for a lumbar disc herniation:
- Intense back pain, often described as persistent, stabbing, and worsening with movement. They also intensify very markedly when the sufferer lifts something or leans forward. The back pain can also be increased by sneezing or coughing.
In many cases, the pressure of the gelatinous core on an intervertebral disc in the lumbar spine area causes pain that radiates over the buttocks into the leg. Patients often complain of a furry numbness. It feels as if ants are running over the leg. We call these sensory disturbances paresthesias.
Muscle tension in the lower back cannot be excluded, possibly paralysis of the leg muscles, intestinal muscles or bladder muscles can occur.
Some patients describe that their reflexes are reduced.
Some people also complain of sudden buckling of the leg.
Cold and warm sensations in the legs that were not there before are also possible.
Many patients perceive a herniated disc in the lumbar spine as a "lumbago", barely able to stand or walk on their heels or toes. Those who do not quickly seek the help of a specialist, but instead fight the pain with painkillers, expose themselves to the risk of additionally suffering from nausea and depressive moods.
What explains the different symptoms?
Two factors determine the exact symptoms of a herniated lumbar spine disc. They determine which restrictions and complaints are present in those affected.
- The level of the herniated disc in the lumbar spine
- The question of whether the leaked material presses on the spinal cord or laterally on the spinal nerves
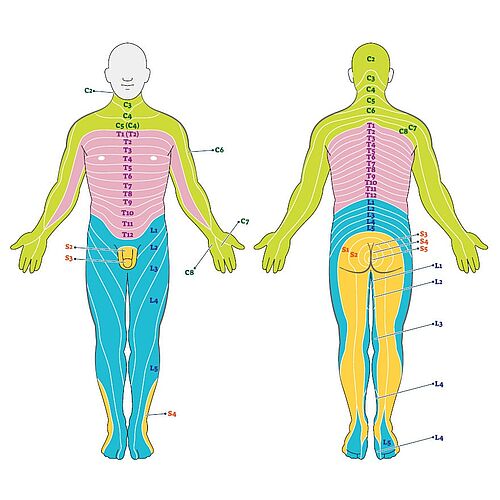
Specialists can already gain initial conclusions about the position of the prolapse by looking at the expressed symptoms. How is this possible? The so-called dermatomes help the specialist to do this. A dermatome is a precisely localized area of skin that is sensitively supplied by spinal nerves of a specific spinal segment. If, for example, fingers tingle and feel numb, if there are deficits in the feet and toes, if gait problems are possibly reported by the patient, then the doctor gets initial indications of the spinal area in which the herniated disc has occurred and is attacking spinal.
Spinal nerves are part of the so-called Peripheral Nervous System (PNS). The main function of this nervous system is to connect the rest of the body with the brain. If the patient complains of deficits that start from the waist and are associated with radiation into the leg, the cause is in the lumbar region.
A more specific example for lumbar spine disc herniations: If a patient complains of numbness, tingling or paralysis radiating down the foot to the tips of the toes, a herniated disc between L5 and S1 is suspected. If a patient reports sensory disturbances, pain and motor restrictions in the hip and buttock area, a higher spinal nerve is probably affected (e.g. L1).
The symptoms of a herniated disc of the lumbar spine are therefore highly dependent on the exact vertebral position. However, with all the knowledge about the dermatomes and sensory disturbances, it must be emphasized: They provide the doctor with initial indications for diagnosis. However, they are in no way a substitute for an MRI examination.
Diagnosis of a herniated disc in the lumbar spine (LS)
In order to treat a disease successfully, the doctor first has to make an exact diagnosis. Without a diagnosis, you can't start a therapy. To make a diagnosis, the doctor uses his medical knowledge, his eyes, his ears, his hands - and the most modern technology available today. These are the imaging techniques such as MRI and computed tomography (CT).
Anamnesis
In order to make a diagnosis, doctors begin with the so-called anamnesis. The word anamnesis (Greek anamnesis = "memory") includes asking and recording the patient's complaints and (suffering) history. In emergencies, the anamnesis is usually very brief to avoid delaying (life-)important measures. In normal situations, we take enough time to take a medical history. The questions we ask are something like these: Where exactly is the pain located? How long have you been in pain? Did the pain come on suddenly, or has it developed? How does the pain feel? Is it sharp, stabbing, dull? Does the pain intensify when you cough, sneeze, make jerky movements? When it is carried? Does the pain radiate to the legs and even the feet? Do you feel numbness or tingling? And if so - where? Occupational and psychosocial circumstances are also considered during the anamnesis.
After the interview, the patient goes to the neurology department, because a detailed neurological examination is necessary. For this, the doctor checks reflexes, sensitivity, mobility and possibly nerve conduction velocity. Depending on whether and where the pain radiates, the doctor can draw conclusions about the level of the spine at which a herniated disc is present. Knowledge of the dermatomes described can also be useful here.
Imaging procedures
The most important imaging procedures are the classic X-ray, magnetic resonance imaging (MRI) or a computer tomogram (CT). The X-ray image provides information about whether vertebral bodies have shifted against each other, what the vertebral structure is like, how large the distance between the individual vertebrae is. At the Avicenna Clinic, we are in the special situation of being able to offer our patients the so-called open MRI. It allows us to comfortably examine even claustrophobic patients or those weighing up to 250 kilograms.
What does the MRI tell us? It helps to distinguish the herniated disc from other conditions that cause similar symptoms. MRI can be used to determine the exact location of the herniated disc in the lumbar spine. A magnetic resonance imaging (MRI) scan shows the specific changes: Herniated disc, its size and exact location, the presence of osteoarthritis, wear, instability and changes in the neural structures (myelopathy) and gives us other important information.
Dr. Munther Sabarini: "We are literally looking inside the body, so to speak!"

Which therapy is used for a herniated disc in the lumbar spine?
Deciding which therapy to recommend for a herniated lumbar spine disc is a big responsibility. Before we recommend surgery at Avicenna Clinic, conservative therapies could possibly help primarily to relieve pain and tension, such as: Drug therapy, injections, computed tomography (CT)-guided injections (PRT), infusions, physical therapy, physiotherapy, manual therapy, osteopathy, electrotherapy and others.
Which therapy is ultimately recommended for a herniated disc of the lumbar spine must be decided on the basis of the following factors:
- Symptoms: Pain, discomfort, loss of strength, and/or bladder voiding dysfunction.
- Success of previous therapies and duration of success, side effects of administered drugs.
- General condition of the patient: severe heart disease, blood thinners?
- Neurological findings: are there sensory disturbances, reflex abnormalities, motor deficits or atrophy?
- MRI findings: small or large prolapse accompanied by tightness, instability?
- Psychosocial factors, occupation, career, care.
A clear recommendation on which treatment concept should be considered can then be provided. This should not only alleviate the symptoms, but also eliminate the cause. After all, the aim is to provide lasting relief from the pain and to prevent further permanent irreversible nerve damage.
Conservative treatment of a herniated lumbar spine disc
Before recommending surgery at the Avicenna Clinic, we discuss conservative treatment of a herniated lumbar spine disc with the patient.
In addition to general rest, conservative treatment includes regular and consistent physiotherapy. We prescribe pain-relieving medications to prevent relieving postures and to ensure that movement exercises are relatively pain-free. In addition, heat applications, fango and mud packs, massages and water temperature can help. They relax the back muscles, which in turn can relieve painful tension. Osteopathy and electrotherapy can have positive effects, CT-guided injections (PRT) can also be useful.
Operation of the herniated disc lumbar spine
Nowadays, a disc surgery is performed microsurgically, that means through a small incision on the back and using a microscope or a camera. The procedure takes about 60 minutes, depending on the location, size and age of the herniated disc. During this procedure, the disc is partially or completely removed. All minimally invasive surgical techniques aim to relieve pressure on the bruised nerve root by freeing prolapsed disc tissue.
Lumbar disc surgery can be performed percutaneously endoscopically (through a narrow tube with optics and a light source) or microsurgically. Minimally invasive procedures include percutaneous laser disc decompression (PLDD) for minor herniations or percutaneous nucleotomy (PN)
With the help of an intervertebral disc cell transplantation, the volume of the intervertebral discs can now be preserved and elasticity restored for the first time - through a biological renewal of the intervertebral disc tissue.
Individual adjustment of the therapy
Which of all these and other methods is suitable in your case will be discussed with you individually during the consultation with the doctor. If surgery is necessary, he will discuss exactly which disc surgery is suitable for you. It is generally known that many herniated disc in the lumbar spine 'takes care of itself' without surgery. However, because surgery is still very common, surgery for a lumbar disc herniation is the most common surgical procedure for the lumbar spine.
The advantages of microsurgery over major classical surgery are obvious to the patient: it provides gentle access, selective exposure of the surgical site, and prevents extensive scarring. It thus gives the patient the greatest possible degree of safety.
Dr. Munther Sabarini: "The success rate of such an operation, which is normally low-risk and without complications, speaks for itself: 95 percent of all those operated experience an immediate improvement in symptoms after the operation. And that is exactly the result that the patient and surgeon want."
When can I return to work and sports after a herniated disc in the lumbar spine?
You will be able and allowed to return to work after a lumbar disc herniation and, of course, to do sports again. Almost any sporting activity is useful after conservative or surgical therapy. The chances of recovery for herniated discs are good as long as the nerves are relieved quickly enough.
As a general rule, patients are allowed to return home a few days after surgery. They should not drive themselves, and should have someone to pick them up. And for six weeks after the operation, the patient must take it easy so that a good healing process can begin in the inner and outer surgical field.
Physiotherapeutic treatments begin while the patient is still in the hospital. Outpatient physiotherapy is usually prescribed, but some patients decide to undergo inpatient follow-up treatment. The advantage of this is that therapists provide personalized care to ensure that the rehabilitation exercises are performed correctly and at regular intervals. Those who do their exercises on an ambulant basis or at home should know that the degree of improvement depends, among other things, on the extent of the herniated disc and its neurological damage. On top of that, discipline and initiative on the part of the patient are necessary and useful.
Exercise helps with the rehabilitation
Movement, movement, movement - this is the magic formula that will quickly get you back on your feet. Hiking, walking, cycling - these are movements that pay off positively during the rehab phase. When walking, make sure you wear good shoes with soft, thick soles to take the strain off your spine. Also: three short walks are better than one very long one! Isometric exercises, which are tension exercises that tighten muscles evenly, will also help you. This activates the segmental stabilizing muscles of the trunk. Showering is already allowed in the first week after surgery, but no tub baths!
If you do not overwork yourself on the one hand and do not underwork yourself on the other during the rehabilitation phase, you will be back at work a good month after the operation. And the pain that made your life difficult will be a thing of the past.
Information about the article
The article was last checked and updated on September 30th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
Sources and further literature
Dt. Ges. f. Orthopädie und orthopäd. Chirurgie + BV d. Ärzte f. Orthopädie (Hrsg.): Leitlinien der Orthopädie. Dt. Ärzte-Verlag, 2. Auflage, Köln 2002.
Jürgen Krämer, Robert Krämer & Jörg Herdmann: Mikrochirurgie der Wirbelsäule. Georg Thieme Verlag KG, 6. Auflage, Stuttgart, 2005.
H.S. Füeßl: Wie sich ein Bandscheibenvorfall ohne Operation zurückbildet. MMW-Fortschritte der Medizin, 158(12), Springer Medizin, 2016.
W. Börm & F. Meyer. Spinale Neurochirurgie: Operatives Management von Wirbelsäulenerkrankungen. Schattauer. 1. Edition, Stuttgart 2008