What is a disc wear?
It is a blessing that intervertebral discs exist. They are the shock absorber, the buffer between the vertebrae. In this way, they give the spine stability and at the same time allow mobility, i.e. movement. Intervertebral discs consist of an outer relatively firm fibrous ring and an inner gelatinous core. The disc cells of the gelatinous core produce structures (glucosaminoglycans) in their environment (matrix) that store water. In the course of life, many loads act on the spine. Due to natural wear and tear, the intervertebral discs lose their buffer function over time. Important fluid needed by the fine supporting cartilage tissue can no longer be stored. Biochemical changes occur in the intervertebral discs, causing them to lose their elasticity and thus their shock-absorbing function. There is a reduction in the number of cells but also changes in tissue quality. Cracks in the intervertebral disc are the natural consequence.
With increasing age, it is normal for heavily loaded intervertebral discs to wear out. In this case, we speak of disc wear. If, however, this occurs beyond the natural level, we speak of pathological disc wear (degeneration). In contrast to a healthy intervertebral disc without its own vessels and without nerve endings, pathological vessels and nerve endings with pain receptors are found in a degenerated intervertebral disc. These changes in degeneration are the basis for further diseases such as: Disc protrusions or herniations, wear of vertebral joints (facet syndrome), spinal stenosis, spondylolisthesis(listhesis) or instability of the spine.
At what age does the degeneration begin?
The process of wear and tear begins much earlier than many patients imagine. Intervertebral disc wear already begins at the age of about 20 years. From the age of 60, changes are noticeable in more than 90 percent of the population. Wear and tear of the intervertebral discs is therefore not a back disease that exclusively affects older men and women. Degeneration of the intervertebral discs can also become a problem at a younger age. Intervertebral disc degeneration can therefore not be limited to a certain age group.
Osteochondrosis or chondrosis?
In connection with the degeneration of the intervertebral disc, two terms are often mentioned that require explanation: Osteochondrosis and Chondrosis.
Chondor meant cartilage, osteo is the bone. This means: In osteochondrosis not only the cartilage is degenerated, but also the bone. We observe in our clinic that osteochondrosis occurs predominantly in the lumbar spine (LS), but it is not uncommon in the cervical spine either. In the thoracic spine (BWS) we observe osteochondrosis only very rarely.
Causes of disc wear
The intervertebral discs lose the ability to hold fluid in the tissue and as a result lose their elasticity. They virtually dry out and can slump. As a consequence, they can no longer dampen the friction between the vertebrae. Back pain and discomfort in the spine are the result.
Causes of intervertebral disc wear can be genetically determined factors, overloading of the intervertebral discs, for example through overweight, lack of exercise, one-sided movement such as long periods of sitting, poor diet or constant heavy lifting or carrying. Occupations at risk are therefore found in the construction and transport industries and in nursing. Here, the back is not protected in daily work.
It is not uncommon for existing impairments of certain spinal segments (herniated discs, stiffening, etc.) to affect other initially healthy segments of the spine. This speeds up further degeneration of the intervertebral discs. Smoking is also considered a cause of earlier disc wear.
Symptoms of degeneration and disc wear
The degenerative changes in the spine are a gradual process. A process that cannot be overlooked because it causes pain. Progressive wear of the intervertebral discs often makes itself felt through the symptoms of back pain and neck pain. Lifting heavy loads and long activities in a sitting position are particularly painful. The severity of the pain increases as the wear progresses.
The resulting instability of the spine leads to a feeling of "breaking in half". The surrounding vertebrae, vertebral bodies and small joints of the cervical spine, lumbar spine or thoracic spine are severely overloaded. Every movement can become torture. The loss of disc height causes narrowing of the nerve exit canal, which can also lead to pain radiating down the leg or arm, tingling and numbness. Turning during sleep can become problematic.
But often pain is not the only typical symptom. Pain is usually accompanied by psychological and psychosomatic complaints. Many sufferers experience mood swings, depressive moods and a general feeling of being unwell.
Diagnosis of symptoms of disc wear
The diagnosis of suspected disc degeneration begins with a conversation, the so-called anamnesis, between the doctor and the patient. In this kind of conversation, facts are collected, such as:
- When did the pain start?
- Where did it start?
- Are there any psychological problems?
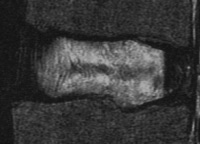
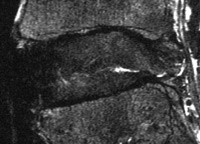
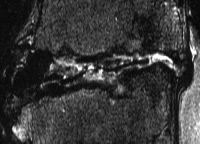
After the conversation and the collection of the medical history, the doctor has a comprehensive diagnostic procedure at his disposal. It may begin with a precise neurological examination. Next, imaging studies detect the status of the intervertebral discs. Here, clinics primarily resort to the diagnostic tools of X-ray examination, computed tomography (CT) and, most importantly, magnetic resonance imaging (MRI) when disc wear is suspected. MRI primarily shows the localization and intensity of disc wear. In addition, the neural structures and the neighboring segments are accurately displayed here.
Treatment with minimally invasive intervertebral disc cell transplantation
The first step in the treatment of pain caused by disc degeneration is considered to be conservative therapy. It includes prescription of painkillers, muscle relaxation, manual therapy, physiotherapy, acupuncture, psychosocial intervention, etc. Active exercises and back swimming are used to strengthen the back muscles, which lowers and reduces the pressure on the disc.
To treat disc wear, the Avicenna Clinic uses minimally invasive disc cell transplantation, in which the worn disc is implanted with biologically multiplied endogenous cells. The implanted cells store more fluid, which brings more elasticity. In orthokine therapy, the body's own substances are injected in higher concentrations into the affected disc and thus they act against the inflammatory changes.
If there is a narrowing of the nerve exit point in the spinal canal (neuroforamina stenosis), microsurgery could widen these exit points or relieve the nerve root. If instability is present, then further treatments such as stabilization, disc replacement, among others, may be considered.
Neurosurgeon Dr. Sabarini: "Disc replacement now has the same status as, for example, hip replacement, which is a standard procedure in surgery today. We in our international spine clinic not only treat patients from Germany with disc replacements, but we also provide disc prostheses to people from abroad, for example from the Arab world."

We always recommend the therapy with the highest chance of success
Complaints can arise from one or more causes. Therefore, when selecting therapy for disc degeneration, many factors are considered, including: Complaints, frequency, success of previous therapies, the presence of deficits, the results of neurological and physical examinations, the results of the examinations performed (MRI magnetic resonance imaging), severity and location of the changes detected (herniated disc, multiple fractures, spinal cord involvement), age of the patient, concomitant diseases, occupation, psychosocial circumstances, and many more. The therapy that is individually suitable for you, with the highest chances of success and the lowest risks, is recommended. Most importantly, the cause of the disc degeneration must be treated, not just the symptoms such as back pain.
How long are patients on sick leave for disc wear?
Of course, when treating a worn disc, there is always the question of how long the patients will be on sick leave. On the one hand, they want to cure the problems in peace, but on the other hand, they are worried that if they stay sick too long, their job will be at risk.
The answer is: the length of sick leave depends on the course of the disease. If the disc wear and tear could be treated quickly, people are fit and at work again accordingly quickly. However, it can also be the case that some patients are absent from work for several weeks because they are simply unable to work, i.e. they are not able to work under sufficient pressure.
Prognosis for disc degeneration
Wear and tear of the intervertebral disc cannot be reversed. Like other parts of the body, intervertebral discs show signs of wear over the course of a lifetime. Depending on the load, they manifest themselves early or late, and complaints are mild or severe.
But there are sufficient possibilities to reduce the progress of the degeneration and to eliminate the pain. Fortunately, patients can do a lot themselves to delay the progress of the disease for a long time. Self-therapies include healthy eating and, if necessary, weight loss. Targeted workouts and exercises also help to stress the body properly rather than excessively.
The following always counts: The pressure on the intervertebral discs must be reduced! Do not lift heavy, do not carry heavy, think about a back-friendly mattress and ideally purchase it. A back school or physiotherapy are helpful factors in the aftercare. Sports are recommended to strengthen the back muscles. Strong back muscles support the spine and its intervertebral discs. Swimming is particularly suitable, as it ideally trains the back and relieves pain in the water. In addition, the body weight does not rest on the intervertebral discs when swimming. Jogging should be taboo because it increases the pressure on the intervertebral discs. Cycling, on the other hand, is ideal.
If possible, avoid wearing support corsets for long periods of time. If at all, corsets should only be used for a short time, because wearing them weakens the muscles. If back pain does return, take a pain pill. Enduring pain sounds honorable, but this creates relieving postures that are not conducive to rehabilitation.
Information about the article
The article was last checked and updated on October, 12th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: