Definition - what is a hemangioma?
Hemangioma = blood sponge. Every one of us has seen such a blood sponge - also called strawberry spot or hemangioma. Since the growth of a hemangioma (embryonic tumor) is not visible on an ultrasound of the baby in the womb, parents are particularly alarmed when their baby is born with a visible hemangioma. Most often, these can be seen on the face or hairline. Ten to 12 percent of newborns are affected by a hemangioma. This makes hemangiomas the most common type of benign tumor in infants.
In fact, such a benign neoplasm of the blood vesselscan occur in several organs. However, they are no longer visible: in bone or lung tissue, in kidney tissue, in the liver, in pancreas tissue (pancreas). Hemangiomas are deformities caused by an excess of tissue proliferating in the veins, arteries or lymphatic vessels.
The hemangioma is a benign tumor that does not cause symptoms by itself. Therefore, spinal hemangioma or vertebral hemangioma is not found in most people. As a rule, it is therefore almost always an incidental finding in the vertebral bodies or in the vertebral arch, which is discovered during a completely different examination. The thoracic and lumbar spine are usually affected. Women are more frequently affected than men. Although such hemangiomas are benign in themselves, they can become dangerous. As they grow, they demand space in the spine, can press on nerves and attack or destroy important structures. They can rarely cause instability with risk of vertebral fractures.
Frequency
These growths of fine blood vessels do not only affect soft body regions such as the skin. They also occur in the bony skeleton. 40 percent of all hemangiomas of the bony skeleton are found in the spine. They are called vertebral body hemangiomas. Such a vertebral body hemangioma can affect the complete vertebra. It is also possible that only parts of the vertebral body are affected. The most common benign tumors of the spine are the hemangiomas with 11 percent.
Causes of hemangiomas
Hemangiomas occur when blood vessels form anew and proliferate in the process, a so-called new formation of blood vessels. The starting point for the formation of new hemangiomas is the cell layer lining the inside of the blood vessels. The exact causes of hemangiomas are not known. Genetic and hereditary factors are possible. Basically, hemangiomas can develop wherever there are blood vessels, i.e. visible externally, but also internally on the organs.
Symptoms of vertebral hemangiomas
The symptoms of a vertebral hemangioma are complex: there is almost always painful restricted mobility in the section of the spine where the hemangioma has settled. Pay particular attention to pressure and tapping pain. A hemangioma can also put pressure on blood vessels, muscles or the spinal cord. Sensory disturbances and bladder and rectum disorders are also possible. Patients also repeatedly report so-called pain at rest. This is pain at a resting position, i.e. without the body being strained in any way.
With malignant tumors, there is often not only pain, but other symptoms - including: Fever, weight loss, night sweats, lymph node enlargement, fatigue.
Diagnostics - how to diagnose a hemangioma?
Most patients who turn to their specialist are perplexed and frightened. They cannot interpret the symptoms. They have no idea of the possible diagnosis. "What is growing in my body?" is a question that doctors are asked again and again. Well, the question cannot be answered immediately even by the best specialist. But he can, in order to name an exact diagnosis, initiate a diagnostic procedure, at the end of it there will be clarity.
As is well known, the very first thing that is needed for a diagnosis is a discussion, the anamnesis, between the doctor and the patient. Here, the patient describes his or her condition and mentions symptoms. It must be conducted in detail and conscientiously by the doctor and the patient so that the doctor receives information that puts him on the right track. After the client has been interviewed, the next steps are those ordered by the doctor. These are usually neurological examinations, ultrasound, computer tomography (CT), magnetic resonance imaging (MRI), laboratory diagnostics, possibly also nuclear medicine examination procedures and a biopsy (removal of a tissue sample).

Therapy - how to treat a hemangioma successfully
Small stable hemangiomas do not require surgery only check-ups. About once a year, an MRI check can show if the hemangioma has enlarged. Kyphoplasty can be used to prevent vertebral fractures. If instability or fracture is already present (both are associated with pain), then the affected segments are stabilized. If the hemangioma has invaded the spinal canal, or if there are already fractured bone fragments in the spinal canal, then these will be removed from the spinal canal by microsurgery.
Such an operation may sound simple in theory, but in reality the removal requires the highest surgical art. After all, the spinal column, with the spinal cord and spinal nerves, is home to vital and extremely sensitive components of the nervous system. During the removal of the vertebral hemangioma, damage to the nerves should not occur under any circumstances. Damage to the nerves is actually always irreparable. As a preventive measure, a hemangioma vertebra can be replaced with bone material during surgery.
Can hemangiomas send metastases through the body?
The question is justified and the answer, to the best of scientific knowledge, is clearly: No. Because hemangioma is a benign tumor, and hemangiomas do not form metastases. The most common benign liver tumor is hemangioma, a new formation of blood vessels in the liver.
Prognosis on vertebral hemangiomas
All-clear for the future, so the prognosis on hemangiomas of the spine is good! One important point, however, remains: After the incidental finding and the following surgical therapy, the patient should accept close medical control for at least one year. The so-called follow-up control takes place in the context of a magnetic resonance tomography and X-ray examinations.
Information about the article
The article was last checked and updated on November, 08th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
Sources and further literature
K. Bohndorf: Radiologische Diagnostik der Knochen und Gelenke. Deutschland: Thieme, 2006.
U. Weber., M. Weyreuther, M. Westphal, C.E. Heyde, J. Zierski: MRT-Atlas: Orthopädie und Neurochirurgie. Wirbelsäule. Deutschland: Springer Berlin Heidelberg, 2006.
I. Wanke, D. Uhlenbrock, M. Forsting: MRT der Wirbelsäule und des Spinalkanals. Deutschland: Thieme, 2009.
T. Kluba: Taschenlehrbuch Orthopädie und Unfallchirurgie. Deutschland: Thieme, 2010.
The Avicenna Clinic in Berlin is always willing to help you
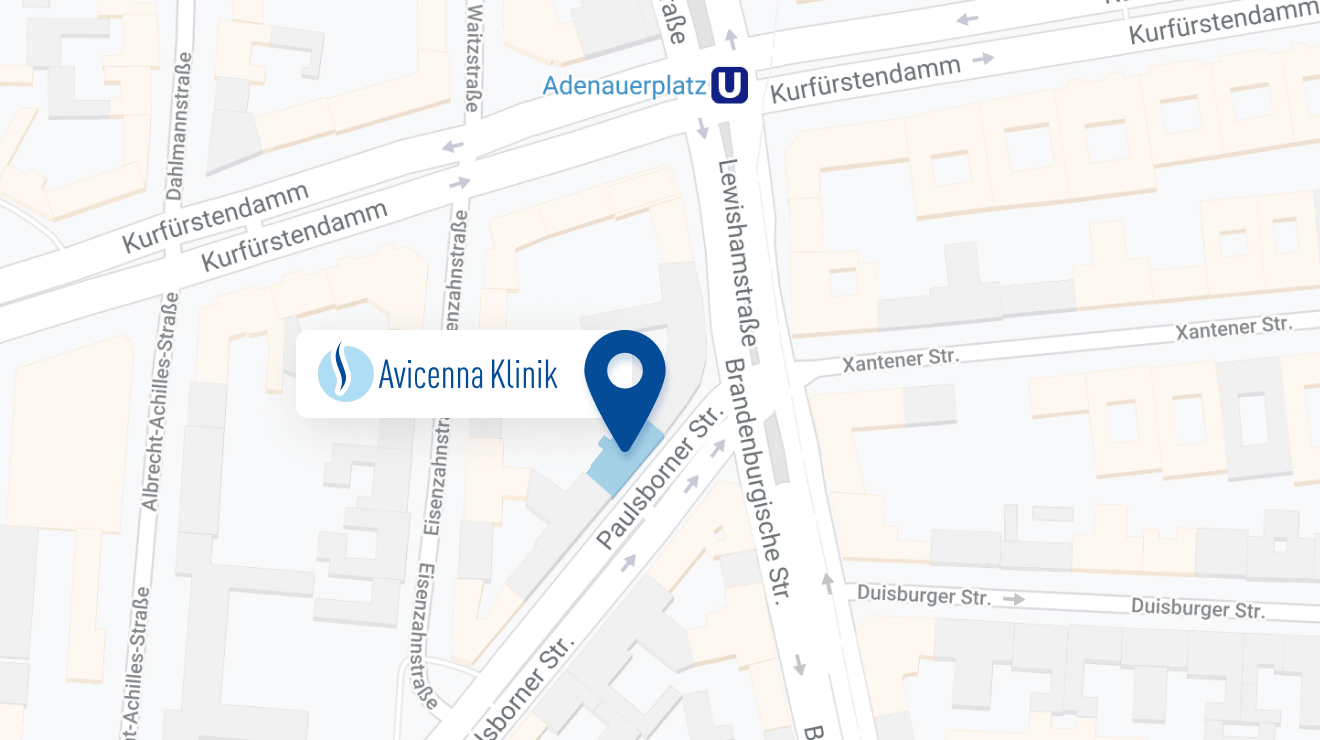
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: