What is myelopathy?
If damage occurs to the nerve tissue in the spinal cord of the cervical or thoracic spine, we speak of myelopathy. The word myelopathy is composed of the ancient Greek components "myelon" for spinal cord and "pathos" for disease or damage. The spinal canal is located inside the spinal column. The spinal cord runs through it, as do the nerve fibers in the lower spinal column. Between the vertebrae, nerves leave the spinal canal and continue to run into the arms, trunk or legs. If there is constant or massive pressure on the spinal cord, then the spinal cord tissue loses its vitality and leads in the long term to the death of the nerve tissue with loss of function. This can be the case, for example, with herniated discs, spinal stenosis, tumors or reduced blood flow. Since the central nerve cells (CNS) in the spinal canal cannot regenerate or multiply, the consequences of spinal cord damage remain forever or worsen.
Depending on the cause of the spinal cord damage in the spinal canal, different forms are distinguished. The localization of the spinal cord damage is decisive for the symptoms. The question is whether the spinal cord of the cervical spine or the thoracic spine is affected.
Frequency of occurrence - men are twice as likely to be affected by myelopathy than women
From experience we know: men are affected by the problem of myelopathy twice as often as women. Degenerative changes in the cervical spine preferentially affect middle-aged and older people. Half of all people over the age of 50 and three quarters of all people older than 65 show signs of cervical myelopathy.
Possibly of interest to you: In a Japanese study, 1155 patients in a county of 2.26 million underwent surgery for cervical myelopathy. Most patients were in their 6th or 7th decade of life. Spinal stenosis was present in 30% of cases. If the nerve roots near the spine are irritated or damaged, the condition is called radiculopathy, also known as root syndrome.
There are several causes for myelopathy
As a patient, you naturally want to know what causes myelopathy. How does narrowing occur in the vertebral canal (canalis vertebralis) with consequences? What are the symptoms of cervical myelopathy? Here are the answers.
Basically, damage to the spinal cord can be caused by various mechanisms and factors. In the vast majority of cases, however, myelopathy is acquired over a lifetime: If the spinal canal becomes too narrowed, significant instability and changes can occur due to such a stenosis. Even leading to deficits and numbness in the arms and legs with disturbance of fine motor skills, sensation, gross strength and gait. Incomplete or complete paraplegia may result if the spinal canal remains narrowed and is not widened.
How can myelopathy be acquired? Narrowing (stenosis) of the spinal cord and the resulting damage to the nerve tracts and nerve roots can result from acute traumatic experiences such as accidents, herniated discs, or falls. This clinical picture is also caused by tissue changes, as in the case of inflammations, but also by tumors or cysts. The different causes trigger different variants of myelopathy.
There are three forms of myelopathy:
- the compression myelopathy
- vascular myelopathy
- the radiation myelopathy
The first one is the compression myelopathy. It can be caused by tumors, spinal and meningeal metastases, post-traumatic e.g. after a vertebral fracture, after herniated discs, by spinal stenosis, spondylosis (wear and tear). In addition to compression myelopathy, reduced blood flow also leads to damage to the nerve cells in the spinal cord. Circulatory disturbances occur with vascular malformations or vascular stenoses. Acute blood loss can also lead to an undersupply of the spinal cord (shock symptoms). If these causes are present, we speak of vascular myelopathy. You have probably heard of radiation damage. Indeed, damage to the spinal cord can occur in the course of radiation therapy. If this is the case, we speak of radiation myelopathy.
Myelopathy - when symptoms develop insidiously
Myelopathy draws attention to itself through various symptoms. They depend primarily on the region of spinal cord damage. The symptoms usually develop with a gradual progression. In cases of pure spinal cord compression, which is usually painless, years may pass from the first symptom until diagnosis. Initial signs may include numbness in the hands or soles of the feet, clumsiness of the hands, and unsteadiness when walking in the dark. For all forms of myelopathy, the damaged spinal cord segments can no longer perform their function correctly in the nervous system, resulting in neurological deficits.
Some patients complain of pain in the neck radiating to the arms or numbness to loss of strength in the arms. Important signs of myelopathy are neurological disturbances. Symptomatic is also falling asleep of the arms or hands during sleep at night. Initial symptoms may include increasing stiffness in the neck with pain when turning the head to the left and right. If there is damage to the myelon, or spinal cord, symptoms may also radiate to the legs and cause unsteadiness in gait and loss of bladder or bowel control. The spinal cord is a pathway of nerve tissue. It carries information from the brain to the body and vice versa. The myelon is located in the spinal canal. Fine motor disturbances in the hands may increase, writing becomes angular and 'spidery', and things may fall out of the hand. It is also harder to button shirts and blouses.
Symptoms of cervical myelopathy (cervical spine)
Cervical myelopathy (cervical means "belonging to the neck or neck part of an organ (cervix)") has a progressive course. At the onset of the disease, there are mild motor (gait disturbances) and sensory functional deficits of the upper and/or lower extremities. Due to unilateral compression, sensory disturbances and progressive motor deficits (Brown-Séquard syndrome) may occur in the extremities (the arm is the upper extremity and the leg is the lower extremity) in cervical myelopathy.
Symptoms of thoracic myelopathy
Myelopathies of the thoracic spine (thoracic myelopathies) have symptoms similar to those typical of the cervical spine. The symptoms occur gradually and result from the loss of function of the respective affected spinal cord areas. Characteristic symptoms include stiffness in the legs, weakness in the leg muscles, difficulty breathing, atrophy of leg muscles, sensory disturbances of the legs and feet, gait disturbances, sensory disturbances, paralysis, bladder and bowel emptying disturbances.
Vascular myelopathies manifest in different functional deficits, depending on the vessel affected. Patients complain of weakness, numbness, impaired fine motor skills, bladder emptying, balance and sexual dysfunction, and muscle stiffness. In advanced stages, tissue atrophy and breathing difficulties may occur.
Myelopathy makes the diagnosis difficult for the doctor
Basically, two things have to be said on the subject of diagnostics:
- An accurate diagnosis is a prerequisite for appropriate therapy.
- The earlier a diagnosis can be made, the sooner a disease is detected, the more favorable the prognosis for a complete recovery. This is obvious, and you may have experienced it yourself. Motto: Quickly recognized - quickly banished!
The diagnosis of myelopathy, on the other hand, makes it difficult for the physician. There is a reason for this: There is no specific early detection sign. In other words, the disease process in myelopathy is often characterized by a gradual and unspectacular course with slow deterioration. As a result, a diagnosis is often not made until the disease has reached an advanced stage. Besides the disease as such, this is the insidious factor about myelopathy.
That is why it is particularly important to use a two-pronged approach to diagnosis. Two-track means conversation and clinical examination. On the one hand, the doctor will ask you about the nature of the symptoms (loss of function, numbness, pain, bladder or rectal disorders). On the other hand, about known previous diseases: Bekhterev's disease, spondyloarthritis, osteoporosis, herniated disc, arterial circulatory disorders or radiation therapy undergone.
In the procedure of diagnosis follows the neurological status with the examination of the gait pattern, the tests for pathological reflexes and for sensory disturbances (anesthesia).
Then comes the use of imaging diagnostics, such as MRI (magnetic resonance imaging). Conventional radiographs can show bony changes well. Additional functional images should always be obtained to determine any instabilities that may be present.
Magnetic resonance imaging is the most important examination method for detecting myelopathy. Myelopathy can be clearly seen in the magnetic resonance imaging slice images. MRI often shows the altered tissue in the spinal cord (brighter than the adjacent tissue). Thus, it is the method of choice for diagnosis. On the one hand, it can be used to see structures compressing the spinal cord, such as a herniated disc or tumors. On the other hand, damaged spinal cord regions can be distinguished from healthy nerve tissue in MRI. The electrophysiological measurements (such as nerve conduction velocity, evoked potentials, etc.) provide important information about spinal cord function.
Usually, the doctor will also order a laboratory test of the blood to detect possible inflammation in the body.
There are different degrees of myelopathy - here is the European Myelopathy Score. See for yourself how you are doing:
The European Myelopathy Score (EMS):
A. Functions of the first motor neuron (gait) | Points |
Inability to walk, help needed | 1 |
On flat ground only with walker/support | 2 |
Climbing stairs only with walker/support | 3 |
Unstable walk, gait pattern appearing plump | 4 |
Normal gait | 5 |
B. Functions of the First Motor Neuron and the Afferent System | Points |
Overflow incontinence, no control | 1 |
Problems of complete emptying and unstable frequency | 2 |
Normal bladder and bowel function | 3 |
C. Functions of the Second Motor Neuron | Points |
Handwriting/eating with cutlery is not possible | 1 |
Handwriting/eating with cutlery is limited | 2 |
Handwriting/shoelace tying awkwardly | 3 |
Normal handwriting/fine motor skills | 4 |
D. Functions of the dorsal horn (Proprioception and Coordination) | Points |
Dressing/undressing only with help | 1 |
Dressing/undressing awkward and slow | 2 |
Dressing/undressing normally | 3 |
E. Posterior roots (segmental radicular paresthesia/pain) | points |
Invalidating pain | 1 |
Recoverable paraesthesia/pain | 2 |
No paresthesia/pain | 3 |
Sum: Division by score | |
Points | EMS degrees |
5-8 | Grade III |
9-12 | Grade II |
13-16 | Grade I |
17-18 | normal |
Myelopathy surgery by microsurgery
If the myelopathy is caused by severe wear and tear (bone attachments), herniated discs, cysts or tumors, then the only way to at least stop the myelopathy is through surgical treatment (microsurgery). The aim of a neurosurgical intervention is to give the spinal cord and nerves more space again by removing or ablating the causes. Several surgical options are available for this purpose:
- If there is a herniated disc, calcifications (spondyloses), tumor, cyst, then these are removed with the help of a special microscope and micro-instruments.
- If spinal canal stenosis is present, then microsurgical spinal canal dilation is performed. In addition to relieving pressure or creating space for the neural structures, replacement of the disc with disc prosthesis or cages (space maintainers) is usually performed. Decompression usually takes place anteriorly.
- In some cases, additional plating, dorsal stabilization, or vertebral body replacement is necessary.
Before surgery, the understandable question arises as to whether complications can occur. Answer: Yes, because complications cannot be ruled out in principle.
But: The risk of a spinal cord injury is sometimes overestimated, often even dramatized. Reality shows: The risk is very low. Injury to a nerve during surgery or postoperative bleeding into the spinal canal is very rare. On the other hand, if surgery is not performed, significant complications arise if the spinal cord remains under pressure or if the myelopathy progresses.
What the patient should expect with cervical spine surgery, for which access is made in the neck, is a few days of hoarseness and difficulty swallowing. Both will pass without needing to be treated.
What happens after myelopathy surgery?
8-10 days after myelopathy surgery, patients are discharged. The day after the surgery, patients are already mobilized. After the surgery, the symptoms will improve, step by step. It has another decisive advantage: it prevents a possible (certain) aggravation.
Back pain? Visit a specialist!
It is always important to listen to your body. So be your own inner doctor. If you take this task seriously - and you should, after all it's about your health - you should know and implement a few things. These include: If you have been experiencing severe back pain in certain areas for a long time, or even a loss of function or discomfort, even gait disturbances, then see a specialist immediately. This should be a spine specialist, a neurosurgeon or an orthopedist.
If it comes to surgery, you should know reassuring - and that is: In about 90 percent of all patients, an improvement occurs. It is most evident, of course, when the condition is detected when symptoms are milder and surgery is performed in a timely manner. Since these state-of-the-art cervical spine surgeries are now performed more gently and quickly, mobilization takes place as early as the day after surgery. The head is supported by a soft tie for one to two weeks.
Also reassuring: at the operated and immobilized level, the disease does not recur.
Measures for prevention
Better than any therapy, of course, is to prevent the disease. Here are a few tips:
- Avoid one-sided stress.
- Avoid permanent bad posture.
- Exercise regularly.
- Strengthen your back and abdominal muscles.
- Seek the help of a physiotherapist even for minor complaints.
- Avoid working with your neck bent for long periods of time, as well as trapping your phone between your head and shoulder.
- When working at a computer screen, you should look as straight ahead as possible.
The Avicenna Clinic in Berlin is always willing to help you
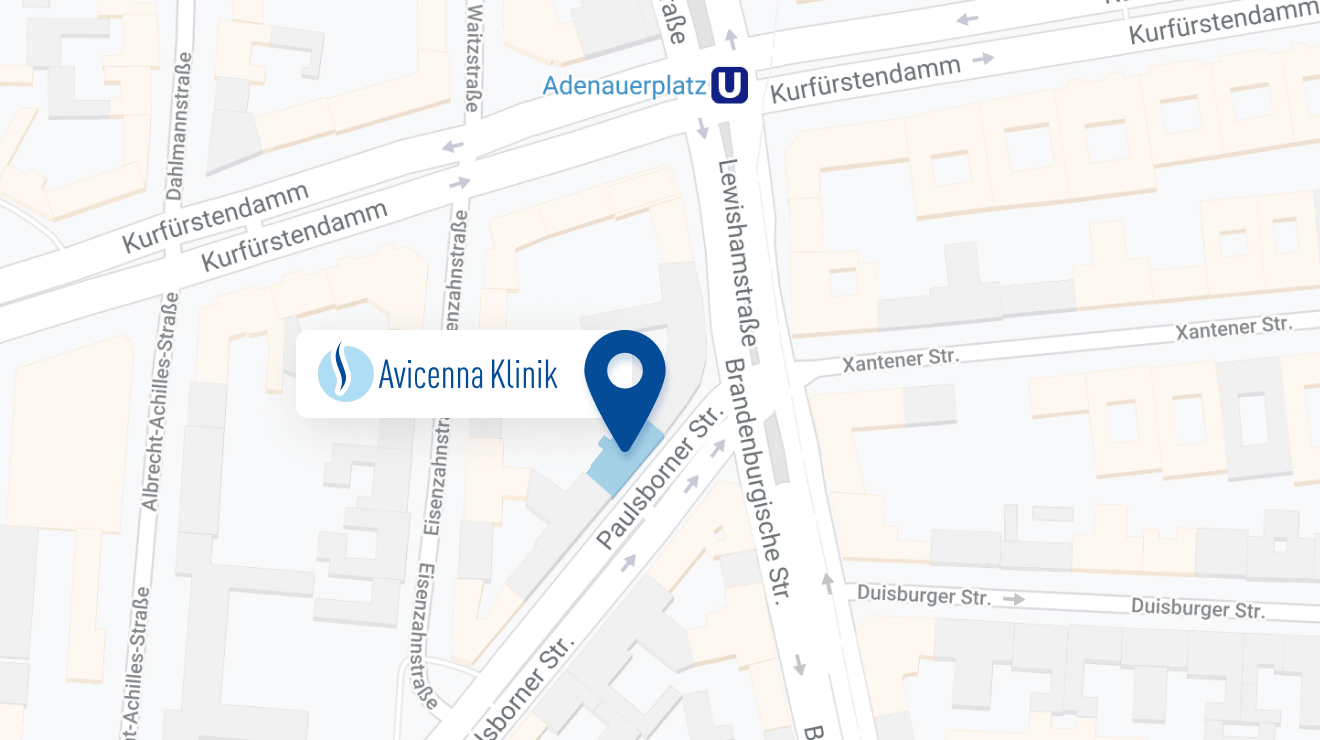
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: