What is post-nucleotomy syndrome?
After spine surgery or disc surgery, we expect elimination or significant relief of discomfort and pain immediately after surgery. Fortunately, this is also true for the absolute majority of cases after surgery. If the pain remains permanently as it was before the spinal surgery, or if it returns, then we speak of postnucleotomy syndrome or postdiscectomy syndrome. In English, it is also called failed back surgery syndrome. About 15 percent of all patients who undergo spine surgery develop postnucleotomy syndrome. The pain often radiates to the arms or legs - even when the surgery was anatomically successful. Preoperative (occurring before surgery) pain remains and returns after surgery.
Reasons for postnucleotomy syndrome
There are several reasons why patients complain of pain despite a "successful" surgery: months or weeks of postponement of a diagnosed and necessary surgery result in permanent and chronic damage to neural structures.
A second reason is severe multisegmental impairment of multiple structures and segments of the spine. Surgery on only one suspicious segment in such a case could lead to only partial success. In some cases, significant scarring occurs, putting pressure on the neural structures. In other cases, the patient lacks individual psychosocial care and support.
In fact, family or professional dissatisfaction or the lack of a suitable job create or manifest a negative atmosphere. Thus, they may be contributors to postnucleotomy syndrome. Pain memory is also thought to be a cause of post-nucleotomy syndrome.
So many people have recurring back pain
Statistically, around 80 percent of people in Germany experience occasional and around 40 percent regularly recurring back pain. A herniated disc alone is diagnosed 800,000 times a year. More than 50,000 of those affected each year require surgery. In 15 percent, symptoms recur.
Postnucleotomy syndrome can occur in a wide variety of spinal surgeries. For example, during surgery due to spinal stenosis or after surgery on one or more intervertebral discs.
Postnucleotomy syndrome symptoms
What symptoms should I look for in postnucleotomy syndrome or postdiscectomy syndrome? The symptoms depend entirely on your individual situation and how you feel. Preoperative pain may remain after surgery, or it may return after some time. Both can be an indication for failed back surgery. The degree of discomfort is similar or even identical compared to the time before surgery.
There are many possible causes for pain after surgery
There are many possible causes for the development of postnucleotomy syndrome:
- Scarring, instability,
- insufficient relief of the nerve roots during surgery,
- in addition, the load on the adjacent segments of the spine sometimes increases after surgery. As a result, they can become overloaded, which can lead to pain,
- psychosocial factors such as strain and stress in private life or at work (see above) can promote the development of postnucleotomy syndrome,
- pain memory. Inadequately treated severe pain eventually leaves traces in the patient's spinal cord and almost certainly in the brain. We call these pain traces "pain memory." This complicated process in nervous life causes pain cells to radio pain signals to the brain, and spontaneous pain then occurs that has no organic cause,
- waiting a long time before surgery, as this can cause permanent damage to the nerve fibers.
Post-nucleotomy syndrome - that is why the diagnosis is important
The search for the reasons and causes of your postnucleotomy syndrome is not easy. On the contrary, it is multifaceted, requires a great deal of specialist knowledge, empathy on the part of the physician, and the sensible use of technology - and you are in demand.
Because, as always, this diagnosis also begins with personal questions, which you should answer as specifically as possible. The questions may be: How and where was the pain before surgery? Where exactly is the pain after the operation? Are they as intense as before? Do you have muscle spasms? Disabling sensations? Can the pain be affected in any way by walking, sitting, pain medication? What therapies have you had so far?
From your answers, your doctor can already get an idea. It is also important that you bring all your medical records with you. This is usually followed by a physical neurological examination. This will include imaging procedures: X-ray, magnetic resonance imaging (MRI), computed tomography (CT). Scintigraphy can be helpful, especially if an inflammatory cause of the pain is suspected. This is a nuclear medicine examination that can be used to assess the metabolism of a tissue.
If the doctor has identified neurological deficits in you, he or she may measure nerve conduction velocity (NLG) for clarification. If a doctor cannot get to the bottom of the problem sufficiently on his own, he will order a so-called multimodal interdisciplinary diagnosis. This means that the final diagnosis is made by a team of physicians (including psychotherapists and physiotherapists). As always, the cause must be researched and identified in order to ultimately help you. And this is what your doctor, in whom you place your trust, is all about.
Possible therapies for post-nucleotomy syndrome
There are various options and combinations of therapies to counteract postnucleotomy syndrome. Optimizing pain management, physiotherapy, CT-guided infiltrations (PRT), facet infiltrations, psychological support, optimizing the workplace - all these procedures can help.
If the pain is predominantly in the lumbar spine (lumbar spine syndrome), cervical spine (cervical spine syndrome), thoracic spine (thoracic spine syndrome), coccyx or ilio-sacral joint area, thermal denervation is a good option. If there is compression on the nerves (recurrent herniation, remnants of an old herniated disc, still existing tightness), reoperation (microsurgery) would be a good alternative. To avoid recurrences, a fibrous ring closure could be a good solution. In such a case, we would apply an anti-scar gel in addition to microsurgery. If there is instability, then stabilization (spondylodesis) is an option.
If there is no clear cause for the pain, spinal cord stimulation would be a good alternative. It offers very good results. Often a combination of several approaches is required.
The right form of therapy or the combination of different reliefs, can only be made after the exact diagnosis by a specialist.
Prognosis on permanent pain after spine surgery
Very important: Do not give your life out of your hands - and life includes not only the present, but also the future. And if you want to create a positive prognosis for yourself after a postnucleotomy syndrome, you are the main player!
Accelerate your freedom from pain or lack of pain by reprogramming your pain memory. Behavioral therapy interventions (such as pain management training, body awareness training, breathing training) can usually help with this. The same applies to physiotherapy measures. In a back school, specifically promote the development of the back and abdominal muscles.
And, what you should know and pay attention to: Postnucleotomy syndrome can gradually turn into a chronic pain syndrome. It is important that these therapies take place promptly for pain after spinal surgery.
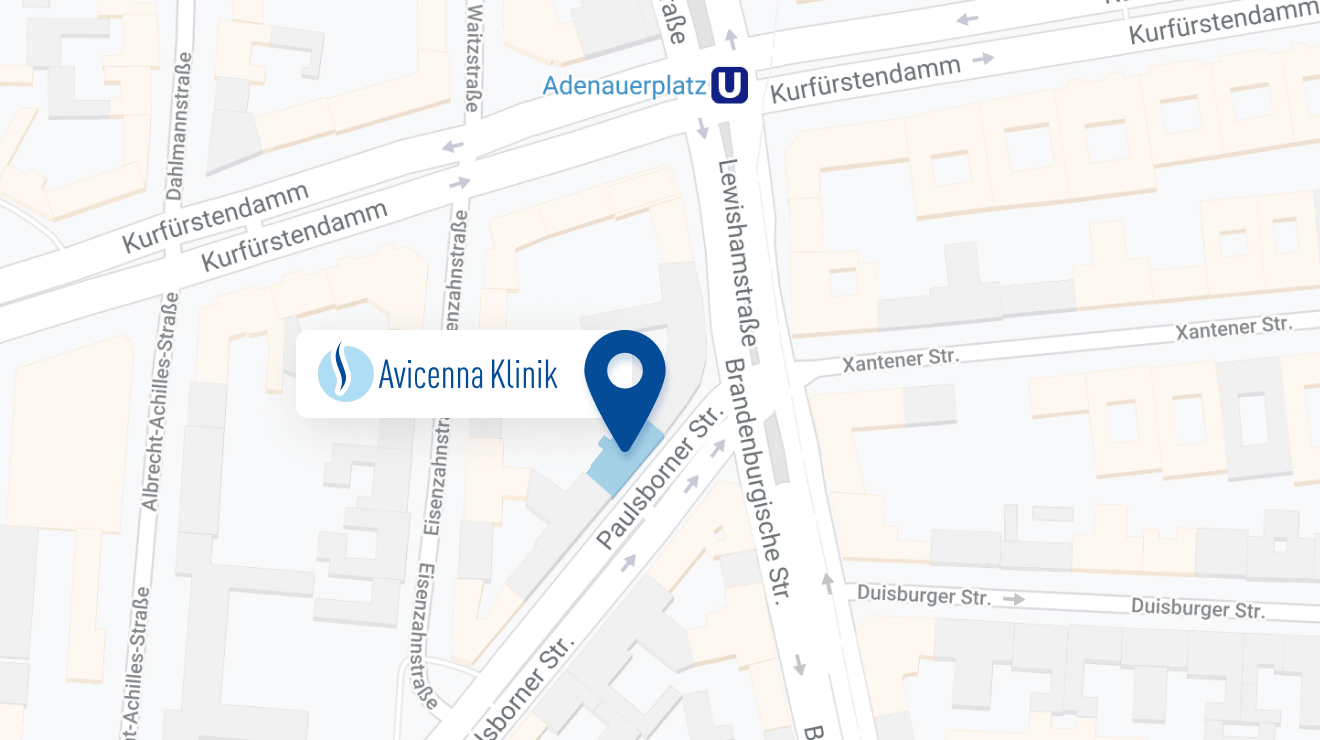
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: