What is a recurrent herniated disc?
Approximately 480,000 lumbar spine surgeries are performed annually in the U.S., mostly to treat herniated discs. The majority of patients subsequently report excellent results. However, in 10 to 15 percent of those successfully operated on, a new herniated disc occurs at the same site, a so-called recurrence (Latin recidere - 'to fall back'). The problems and complaints of the intervertebral disc return.
In this case, affected persons feel pain again despite previous surgery and suffer a relapse. They resemble the pain before the first operation. The symptoms of these repeated disc herniations after surgery are also similar. The pain radiates back into the leg, and neurological deficits (numbness) may also occur. Some patients even report that the pain is more severe than the first herniated disc. This is caused by scarring in the area of the nerve root resulting from the first surgery. Recurrences usually occur months or years after the first operation - very rarely earlier.
Causes of a repeated herniated disc
Because the operation has not brought any lasting improvement, patients, but also surgeons and treating physicians, are very disappointed. In this context, recurrences do not usually occur due to incorrect patient behavior or incorrect surgical technique. The causes of a herniated disc recurrence lie here:
- In the progression of the wear process of the disc.
- In the still existing muscle weakness around the spine.
- In insufficient therapy of the back after surgery.
- In premature strains. In fact, some patients who have undergone surgery make the mistake of putting too much strain on their discs too soon (including heavy lifting and carrying).
- The surgical technique also plays a certain role - whether it was performed microsurgically or according to traditional methods. Some authors explain a new herniated disc by the fact that the tear in the fibrous ring is still open. The fibrous ring tear represents a "gateway", so to speak, through which disc tissue or the gelatinous core can escape again.
Diagnosis of herniated disc recurrence
If you have been "successfully" operated on a herniated disc, but your discomfort and back pain have recurred, then you should see your doctor. Only he can determine whether there has been a repeated herniation of the disc. Medical technology helps in making an accurate diagnosis.
Your surgeon will certainly first order an MRI (magnetic resonance imaging) of the operated spinal area. Here, contrast material is put in to distinguish between postoperative scarring (spinal adhesions) and recurrence of herniation. Scar tissue absorbs contrast material, while newly prolapsed disc tissue does not. If the prolapse occurred several years ago, contrast medium can be omitted because the radiologist can then distinguish a new prolapse from scarring even without contrast medium.
In patients with a pacemaker and similar electromagnetic devices, a CT (or CT myelography) is ordered.
The MRI then shows whether a new prolapse is present and allows conclusions to be drawn about the exact size and location of the recurrence. In this way, it is possible to examine exactly what is going on in the back and whether there is in fact a recurrent herniated disc.
Therapy of herniated disc recurrence
A second herniated disc has actually occurred in the same location. What is to be done now?
Based on the complaints, the neurological findings and the MRI results, a therapy plan will be discussed with you. Of course, conservative therapy (pain medication and physiotherapy) will be sought first. CT-guided PRTs (injections) might also help relieve the pain for a while. If the discomfort is more in the cervical, thoracic or lumbar spine, thermo-denervation could be applied. If there is a new protrusion, then laser disc decompression (PLDD) could be considered.
Is a new disc surgery necessary?
The decision for a new disc surgery (microsurgery) to remove the "new" herniated disc is made if the above therapies have not helped or if they can not be applied. The surgical procedure is the same as the first operation - with the difference that there are often adhesions and tissue that are removed. The inpatient stay after this disc surgery is around 5 days.
Removal of the disc as an option?
There is, of course, the consideration of removing the entire disc, but this is not an easy decision. Why? Because it carries risks that need to be considered for the future.
The problem is that if the disc is missing, this accelerates the degeneration of the adjacent vertebral edges. In the long term, this surgical approach often causes significant deterioration and results in further surgery later and, in the worst case, spinal fusion. A replacement for the intervertebral disc (disc replacement - artificial disc, or placeholder (cage)) also means more or less a stiffening of the segment. Artificial discs in the lumbar spine (high-risk abdominal approach) also often stiffen after a few years.
Medical professionals have known about this problem for years. One solution is to close the tear with a so-called titanium plugger. If the patient decides to do this, he must be informed of the risks, which should not be underestimated. This means that the implant can slip and injure nerves in the process. Also to be considered: the creation of unclear MRI images due to the formation of shadows, the so-called artifacts, in the event of a repeat MRI.
There is an alternative to close the tear of the fiber ring with a stable special thread.
Are recurrences to be avoided?
Is there a one hundred percent way to avoid recurrences?
Clear answer: Yes and No!
However, we assume that timely and correct mobilization after the first operation and correct postoperative follow-up are the best therapies to prevent recurrence.
Of course, the patient also has a great responsibility to remain pain-free. This means that despite excellent results after the first operation, he should approach his life carefully and refrain from early exertion. It is also important to strengthen the back muscles slowly but continuously.
Prognosis to the repeated herniated disc
Why is the fear of a third recurrence usually unfounded? Why does a third incident almost never occur?
The answer lies in the experience of the second recurrence. It has set all the alarm sirens ringing and heralded a new behavior. These mostly younger disc recurrence patients have mostly well-preserved discs, and they are willing to strengthen their back muscles. However, should a new prolapse occur, this is not a downfall either: effective therapy with targeted physiotherapy is always possible. Inpatient rehabilitation is usually not necessary. The recovery process can be accompanied by regular check-ups.
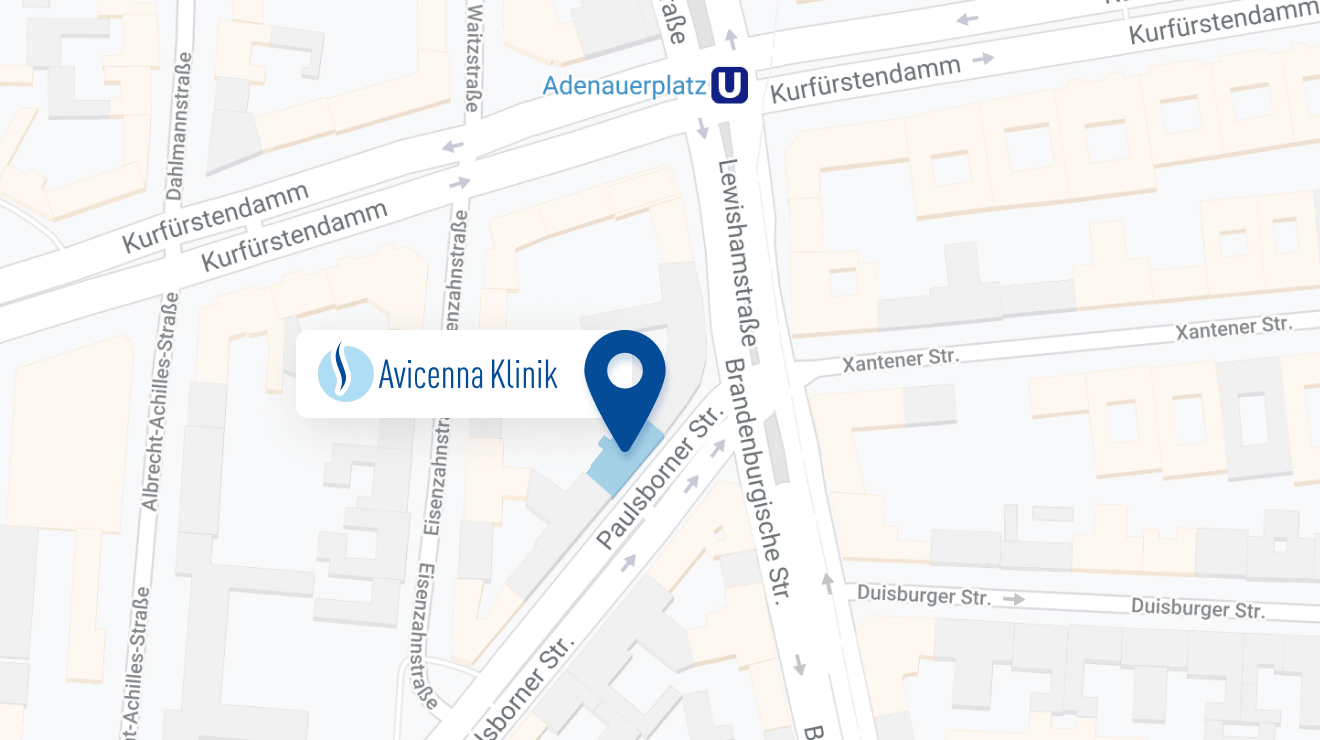
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: