What is a spinal canal stenosis?
Inside the spine is the vertebral canal - the spinal canal. The spinal canal is something very special in the body, something important: it protects the spinal cord and the emerging nerve roots. The structure of vertebrae, intervertebral discs and ligaments encases the soft spinal cord and the nerves that run to the arms and legs. Spinal canal size varies by age and gender. As a guide, a diameter of 25 mm is common in the cervical spine and 30 mm in the lumbar spine.
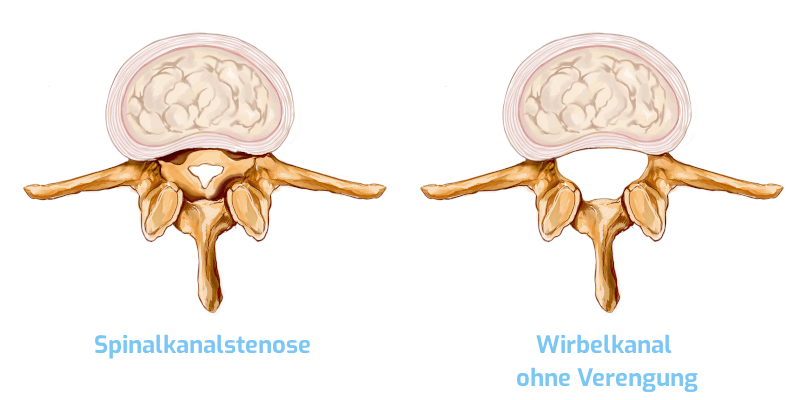
When there is a narrowing (stenosis) of the spinal canal, it is called spinal canal stenosis. In such a spinal stenosis, the spinal canal becomes narrowed due to the deposition of calcium or bony attachments and/or thickening of the ligaments. The graphic below clearly shows what a spinal canal with a stenosis looks like.
What does intermittent claudication mean?
Often, a narrowing in the nerve exit hole (neuroforamina stenosis) is found in combination with spinal stenosis. The term "intermittent claudication (shop window disease)" has arisen from the fact that affected persons experience pain after a short period of physical activity due to the lack of oxygen. Because of this pain, the affected persons have to stop their current activity for a short period of time. However, so that other people do not notice the discomfort, for example when shopping, patients often stop in front of shop windows until the discomfort subsides. Spinal stenosis can lead not only to back pain but also to permanent nerve damage due to pressure on the spinal cord, nerves and blood vessels.
Women are more often affected by spinal stenosis than men
80 percent of all people in Germany suffer from occasional back pain, 40 percent suffer from permanent pain. There are radiological signs of spinal stenosis in about 20 percent of all people over the age of 60. Women are more frequently affected than men (ratio 3:1). Approximately 60,000 patients with spinal stenosis require hospital treatment each year. A distinction must be made between congenital and acquired spinal stenosis. Congenital stenosis is a rare form of narrowing.
Causes of the spinal canal stenosis
How does spinal canal stenosis occur? In the process of aging, a gradual narrowing of the spinal canal happens in almost all people. Most often, the spinal canal is narrowed at the level of the lumbar spine (lumbar spinal stenosis), more rarely in the area of the cervical spine (cervical spinal stenosis). With increasing age, the intervertebral disc has less and less water content. As a result, the intervertebral discs become flatter, tear more quickly, and become more unstable. These changes lead to the formation of reactive bone spurs and the protrusion of some ligaments into the spinal canal. In this way, a slowly progressing narrowing of the spinal canal occurs.
Can the slowly progressive bone constriction of the spinal canal be reversed by targeted physiotherapy? Unfortunately no, but the discomfort can be reduced if regular physiotherapy with appropriate exercises is performed.
The main symptoms of spinal stenosis - these include tingling and numbness.
In spinal canal stenosis, leg pain (with a feeling of heaviness and cramps) is usually the primary symptom. Some patients have additional back pain. Very often, the symptoms occur mainly when walking and/or standing. Leaning forward or sitting down reduces the discomfort or makes it disappear altogether, as this posture widens the spinal canal and briefly relieves pressure from the nerves in the spinal cord. Patients who have lumbar spinal stenosis usually also complain of numbness, tingling, weakness and heaviness in the leg. They may also experience weakness, limited range of motion, sleep disturbances, bladder emptying problems and erectile dysfunction. If the spinal canal of the cervical spine is narrowed, arm pain occurs, as well as insensations. As the condition progresses, weakness of the arms, unsteadiness of movement, and other symptoms may occur, as in cervical myelopathy. The symptoms of spinal stenosis increasingly restrict the everyday life and quality of the affected person.
Surgery for stenosis of the spinal canal? Before therapy, a diagnosis is usually made by MRI
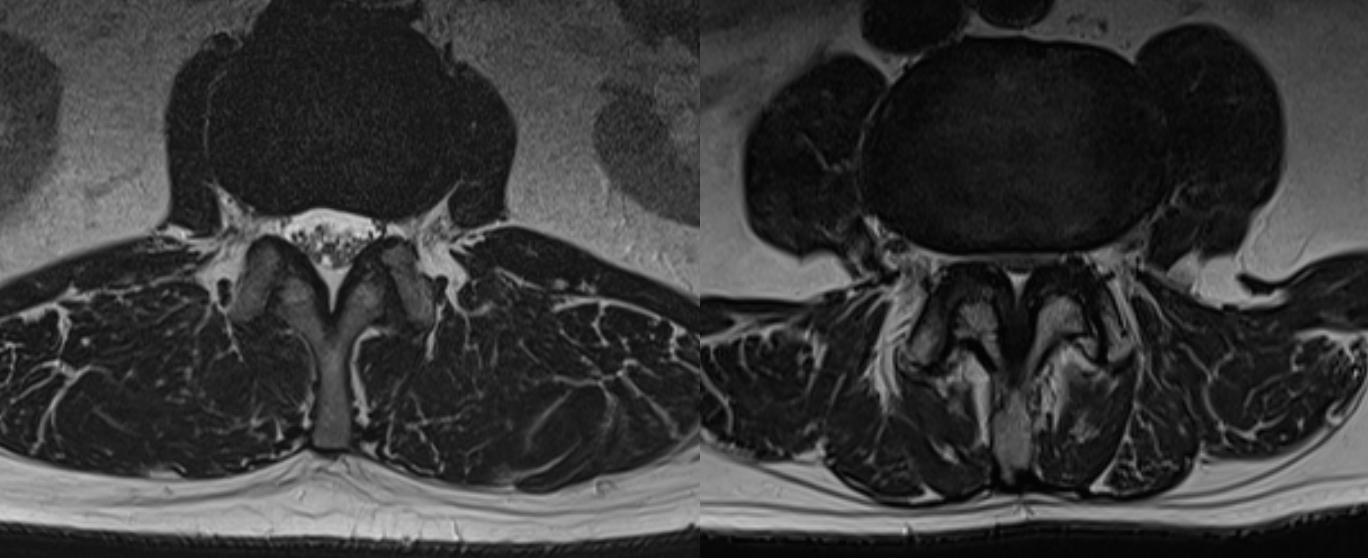
Before a therapy for back and leg pain, a detailed anamnesis (in-depth patient interview), a physical and neurological examination and additional radiological examinations of the patient by specialists are necessary. To make a definite diagnosis, the medical image used is magnetic resonance imaging (MRI). An MRI can show nerves, intervertebral discs, blood vessels and other structures in great detail in slice images. A slight but broad disc protrusion can often be seen as well. Computed tomography can also show the bony changes particularly well. Because of the radiation exposure, this examination method is predominantly replaced by magnetic resonance imaging - MRI). A functional X-ray of the lumbar spine is necessary in a flexed and an extended position of the patient in order to simultaneously diagnose or exclude an instability of the spine, the so-called spondylolisthesis (vertebral slippage). If the diameter of the spinal canal is less than 15 millimeters, we speak of relative spinal stenosis, and less than 10 millimeters - of absolute stenosis.
Treatment options for spinal canal stenosis - is stenosis curable?
Only after careful diagnostics we decide which therapy is to be applied in each individual case and draw up an individual treatment plan. This includes painkilling and anti-inflammatory drugs, injections, physiotherapeutic exercises and physical therapy measures. However, in some cases it is advisable to dispense with conservative therapies if they are not feasible due to individual findings or if there is an exacerbation of the stenosis or symptoms or failures.
Is spinal canal stenosis curable?
For patients with clear symptoms, a wait-and-see attitude is not advisable, as they are increasingly weakened by the restrictions and have less and less condition. We recommend surgery if the problems (insensations, reduced strength and bladder emptying disorders, problems with defecation) can no longer be alleviated with conservative measures.
Spinal canal stenosis surgery
Spinal stenosis surgery is a routine procedure with a low complication rate. Surgery under general anesthesia is considered a routine procedure with a low complication rate, but of course spinal canal stenosis surgery is a technically demanding procedure. Such an operation should only be performed by a specialist and considered by the patient as the therapy of choice.
Microsurgery has been very successful as a treatment option. In this surgical method, the pinched nerves are relieved by removing the calcifications and thickened structures. In this way we widen the spinal canal and the neuroforamen. If the lumbar spine is also unstable, then spondylodesiswould be an option.
In contrast to conventional surgical procedures, microsurgery requires only a small incision of about 3 centimeters per segment. This significantly reduces the risk of subsequent scar formation. With microsurgery, stability is hardly affected, in contrast to conventional methods. Conventional surgery usually involves extensive bone removal. This impairs the stability of the affected segments and makes accompanying spinal fusion necessary.
Microsurgical widening of the spinal canal creates more space, and so the neural structures can recover or regenerate. Against scars we use an anti-scar gel. Now you can strengthen and stabilize your back muscles. Your stable muscles prevent new development of neural stenosis.
Prospects of success and complication rate
Of course, patients at the Avicenna Clinic ask about the prospects of success before the operation. Our answer is: almost always the surgery shows an immediately effect, in eight out of ten people we observe a significant improvement in the long term. Since the procedure has an extremely low complication rate, the operation is also a sensible therapy of choice for patients of advanced age - between 70 and 90 years.
Prognosis: What can I do after spinal stenosis surgery? And what should I avoid?
The surgical suture heals very quickly and is hardly visible after a short time. The wound after spinal stenosis surgery, however, must heal well not only externally but also internally. That is exactly why it is important that you take it easy physically in any case for the first six weeks after the microsurgical procedure.
The return to normal everyday activities must therefore be gradual. Longer walks are possible shortly after discharge from the Avicenna Clinic. Light swimming is allowed after three weeks, but you should refrain from heavier exercise or heavy lifting for at least six weeks. Rotation and flexion of the spine must always be performed with care.
In any case, it makes sense for us to write you a prescription for back training or physiotherapy for the period after your hospital stay. Our recommendations include, for example, muscle-relaxing massage procedures, heat therapy, lymphatic drainage, baths, mud and fango packs, electrotherapy or exercise therapy. In addition, muscles need to be strengthened and patients should learn to adopt a back-friendly posture in everyday life.
Of course, the question "When can I go back to work?" is always an important one. The answer depends on the profession. Those who work hard physically have to take a longer break than those who work at a desk. As a general rule, the period of incapacity for work is between four weeks and three months.
Recognize spinal canal stenosis early
Good news for all those who are afraid of spinal canal stenosis: Spinal stenosis is a slow process that can be stopped in many cases with special training. One of the everyday tips from doctors and physiotherapists is to ride a bicycle, which gives your nerves more space again. You should sit down and bend forward when your legs don't want to go any further. And keep in mind in everything you do or don't do: Abdominal and back muscles support your spine. However, tension and back pain are hard to prevent if your muscles are untrained. Then tension can cause pain that feels like a stenosis in the spinal canal - but has nothing to do with it.
Where do you have pain when you have spinal canal stenosis?
Pain in one or both legs is the classic pain in spinal stenosis. Back pain in the lumbar spine tops the list. Primarily, the pain is felt while walking, standing, and sitting up straight.
Leaning forward or sitting down reduces the discomfort or it disappears altogether, as this posture widens the spinal canal and briefly takes pressure off the nerves in the spinal cord. With spinal stenosis in the cervical spine, you are also specifically affected by neck pain.
Is spinal canal stenosis dangerous?
Normally, spinal stenosis is not dangerous. Without treatment, in the worst case failures can develop with weakness and gait disturbances as well as problems with urination.
How do I sleep properly with spinal stenosis?
For a good sleep despite spinal stenosis, you influence what is possible. This starts with the room temperature - it should ideally be around 18 degrees.Prevent drafts, alcohol, and if possible, stress and mental loads.
Make sure you have a good mattress. It should not be too soft and not too hard. Ideal is a point-elastic mattress, which optimally supports the body shapes especially in the area of the shoulders and pelvis. The pillow that supports the head and spine should not be too large.
As a general rule, restful sleep is necessary to enable regular regeneration of the entire organism, including the intervertebral discs and trunk muscles. You cannot significantly influence the changes in your sleeping position during the night, but when falling asleep you should make sure that you lie on your side with your knees slightly bent. This allows the spine to lie in its natural curvature. Falling asleep in the abdominal position is poison for the cervical spine.
What other symptoms can occur with spinal canal stenosis?
Other symptoms of spinal stenosis may include tingling, weakness and numbness in the legs. Urinary and fecal incontinence and erectile dysfunction..
Very often there are restricted movements, among other things, when writing, buttoning a shirt or blouse, grasping objects (e.g. knife and fork). Stressful and typical are gait disturbances.
Symptoms express themselves differently and also change whether you are in the early stages or in a further stage of stenosis.
Should I be afraid of spinal stenosis surgery?
Microsurgery has been very successful as a treatment option, and the risks for complications are generally much lower than with open surgery. In this surgical method, the pinched nerves are relieved by removing the calcifications and thickened structures. In this way, we widen the spinal canal and the neuroforamen (exit hole of the nerve root). Otherwise, nerves could suffer irreparable damage from constant pressure. Small forceps are used to spare soft tissue, and high-speed burrs are used to work on the bone.
Afraid of surgery?Such an operation is now a routine procedure, but one that allows great improvement. And by using the surgical microscope, all nerve structures can be seen and thereby protected.
Patients are allowed to walk and stand already one day after the operation. After 8-10 days at the latest, the stenosis surgery patients are allowed to go home. Most patients are between 65 and 75 years old. In principle, however, this operation knows no age limit. After all, people in the second half of life also have a right to quality of life.
The most common cause of spine surgery on patients over 60 has now become spinal canal stenosis of the lumbar spine.
What should be avoided with spinal canal stenosis?
Very important: You should not ignore the first signs of spinal stenosis, instead you should take them seriously. Nothing is worse than looking away. Don't fill yourself up with painkillers forever in the hope that it will eventually get better. This way you are only treating the symptoms, and the painkillers will have to get stronger and stronger.
In other words, go see a specialist - they will examine you and work with you to come up with recommendations that may eventually lead up to an operation.
Can I prevent a spinal stenosis?
A spinal stenosis is a gradual process. It usually takes a period of several years. Therefore, spinal stenosis is difficult to prevent, especially since there are hardly any symptoms at the beginning. And yet, there are a few good everyday tips to delay stenosis..
One tip is to stay active with sports, because abdominal and back muscles support your spine. Ride a bike, which gives your nerves more space again. You should sit down and bend forward when your legs don't want to go any further.
It also makes sense to pay attention to weight, or reduce it at an appropriate time. Why? Because overweight increases body posture, so that the narrowing of the spinal canal becomes effective more quickly. If the body has to carry more, it can lead to faster decrease and wear of the lumbar spine.
What is helpful for spinal canal stenosis?
Conservative therapies can be a good start for treatment - especially for mild stenosis. These include painkilling and anti-inflammatory drugs, injections, physiotherapy exercises and physical therapy measures. Physical therapy is primarily about exercising the muscles of the back and abdomen. Strong muscles stabilize the back and can take pressure off the spinal structures. Relaxation techniques can also be useful to improve muscle cramping. With all that being said, unfortunately, don't fool yourself: The progressive bony narrowing of the spinal canal cannot be reversed even by the best physiotherapy.
Ultimately, the cause of the discomfort must be successfully treated: If pain can no longer be resolved with conservative methods, or if there are already deficits, we recommend microsurgical widening of the spinal canal, known as decompression with a surgical procedure. At some point, waiting, delaying an operation does not make sense. Because over time, the spinal canal does not become wider, but only narrower.
What causes spinal canal stenosis?
Degeneration and wear are the main causes of spinal stenosis. If you look at imaging such as magnetic resonance imaging (MRI) before therapy, 90 percent of the time you will see degeneration of the discs.
But there are other degenerative conditions that can cause or exacerbate spinal stenosis. These are:
- Disc protrusion (bulging of the intervertebral disc)
- Herinated disc
- Osteochondrosis (a degenerative disease of cartilage and bone caused by wear and tear)
- Spondylarthrosis (facet joint arthrosis)
Information about the article
The article was last checked and updated on August 31th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
Sources and further literature
- Karla Schildt-Rudloff & Gabriele Harke. Wirbelsäule: Manuelle Untersuchung und Mobilisationsbehandlung für Ärzte und Physiotherapeuten. Urban & Fischer Verlag. 7th edition, München 2021.
- Dt. Ges. f. Orthopädie und orthopäd. Chirurgie + BV d. Ärzte f. Orthopädie (Hrsg.): Leitlinien der Orthopädie. Dt. Ärzte-Verlag, 2nd edition, Köln 2002.
- Jürgen Krämer, Robert Krämer & Jörg Herdmann: Mikrochirurgie der Wirbelsäule. Thieme Georg Verlag, 6th edition, Stuttgart 2005.
- J. Beyerlein. Die Spinalkanalstenose – ein Überblick. manuelletherapie 2018, Issue 22.
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: