What is cerebrospinal fluid loss syndrome?
The CSF loss syndrome, or the leakage of CSF, is less noticeable when the patient is lying down, and much more noticeable in an upright position. The consequences of the disease are enormous: it ranges from an easily endurable headache to an unbearable headache. Many patients are then actually unable to get out of bed or move their head in many cases. Vomiting, nausea, irritability, visual disturbances and others are also possible. But what exactly is cerebrospinal fluid loss syndrome?
We know: About 150 milliliters of nerve fluid (called CSF) surround our brain and spinal cord. The cerebrospinal fluid is located between the meninges and the spinal meninges. Cerebral membranes and spinal cord membranes (dura) literally pack this closed system watertight. If the skins are not tight, neural fluid can leak out. Even a tiny tear leads to sudden and rapid loss of neural fluid from this closed space, with sometimes dramatic consequences.
Cerebrospinal fluid leak syndrome has several names and synonyms: cerebrospinal fluid leak, hypoliquorrhea, spontaneous spinal fluid fistula, intracranial hypotension syndrome, orthostatic headache syndrome, spinal headache, and others.
CSF loss syndrome affects women more often than me
CSF loss syndrome is certainly not a widespread disease, but it is also anything but an exotic rarity. Every year, between 5,000 and 6,000 people are diagnosed with the disease. Women are more frequently affected than men: for every case in a male patient, there are two women suffering from a CSF leak and leaking cerebrospinal fluid. On average, patients are around 40 years old when the disease occurs.
The cause of a cerebrospinal fluid loss syndrome is in the back
The cause of the loss of the cerebrospinal fluid and the negative pressure that results can be a sharp edge (bone spur) on the spinal column. It virtually bores a hole in the spinal cord skin, which actually protects the cerebrospinal fluid. For example, wear and tear can be responsible for a bone spur when joints or vertebrae rub against each other. This leak of the cerebrospinal fluid space is predominantly located in the thoracic spine or the lower cervical spine and ultimately leads to cerebrospinal fluid hypotension syndrome.
Sometimes, after a (minor) trauma, there may be a small tear in the spinal dura, leading to CSF leak syndrome. So the cause is in the back, but complaints and symptoms are in the head.
Another cause of CSF hypotension syndrome is a leak after diagnostic CSF puncture. It develops within 24 hours in 65 percent of patients. Many times, symptoms of the condition may even appear within 20 seconds. The syndrome can develop after spinal anesthesia and during or after spinal surgery.
These are the symptoms of a cerebrospinal fluid leak
The cardinal symptom is the so-called orthostatic headache. It is triggered or aggravated by a change of posture to the upright position. The brain is displaced downward, causing traction on pain-sensitive structures.
Independently of this, there may be other symptoms of cerebrospinal fluid hypotension that improve only when the patient is lying down:
- Nausea, vomiting
- Neck stiffness
- impaired consciousness, impaired concentration and increased pulse rate
- threatening bleeding
- Hearing impairment: tinnitus, hearing disorders, hearing loss, sensitivity to noise
- Impairment of vision: sensitivity to light, double vision, visual and visual field disorders
- Balance disorders: Dizziness, unsteadiness of movement
Occasionally, pain between the shoulder blades or in the neck precede the actual headache by days to weeks.
Diagnosis of cerebrospinal fluid loss syndrome
If a cerebrospinal fluid loss syndrome occurs as a result of a diagnostic puncture of the cerebrospinal fluid space (CSF puncture), after spinal anesthesia or after spinal surgery, the diagnosis is relatively simple. It can be assumed with a high degree of certainty that the loss of cerebrospinal fluid or neural fluid is a direct result of the procedure.
The situation is different if the patient comes to the clinic in pain with no apparent intervention. If something indicates cerebrospinal fluid loss, an MRI (magnetic resonance imaging) scan of the head to the sacrum is ordered for examination. With the help of this imaging technique, it is possible to identify what the underlying cause is. In this way, it can be determined if the diagnosis is actually cerebrospinal fluid loss syndrome.
Therapy and healing of a cerebrospinal fluid leak
To achieve a cure of a CSF leak, patients have four levels of therapy at their disposal:
- Stage 1: Bed rest, at least three days.
- Stage 2: Blood patch: The doctor takes blood from your vein, then injects it into the so-called epidural space. Usually, this method helps to take away the patient's pain permanently. This application of a blood patch can be repeated several times if necessary.
- Stage 3: In principle, the same procedure as for a blood patch - with one difference: the patient's own blood is injected exactly where the dura fistula is located, under X-ray and control by CT. The intervention with a special needle should lead to scarring and consequently to a closure of the CSF leak.
- Stage 4: Surgery: The CSF fistula is surgically closed during a microsurgical procedure. Surgery is only performed if the CSF leak has not closed despite bed rest and a blood patch - i.e., in the case of larger fistulas and pronounced symptoms.
Important: Before the procedure, you should talk to the doctor so that he can inform you about possible risks (e.g. post-operative bleeding, nerve injury, infection).
Positive prognosis after the loss of the nerve water
The acute phase around a CSF loss syndrome is often painful to very painful. After successful therapy, you can live your life as you did before! Once the dural fistula is closed and the brain and spinal cord are once again well embedded and protected in about 150 milliliters of CSF, nothing stands in the way of a positive prognosis.
Information about the article
The article was last checked and updated on October, 31th, 2022
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
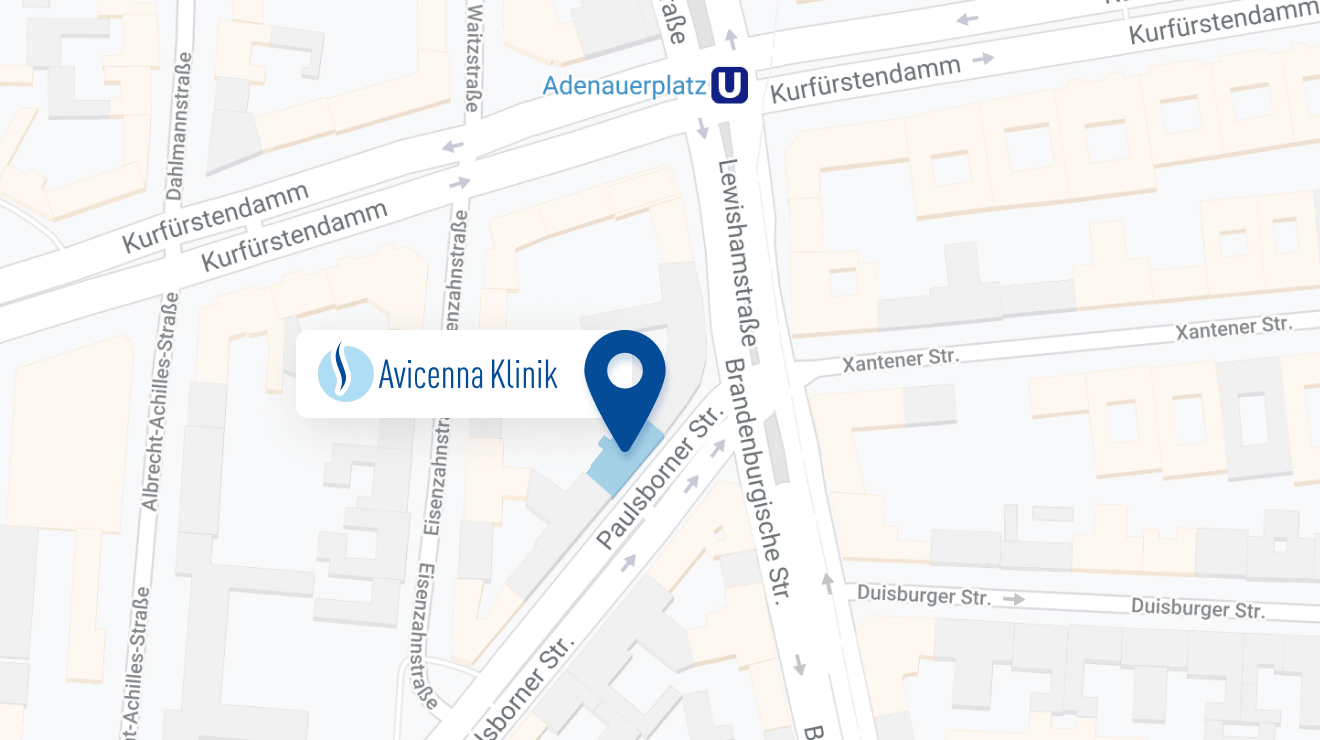
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: