What tasks does the thoracic spine have?
It is well known that in the cervical and lumbar spine, a herniated disc and a spinal stenosis (wear, degeneration of the spine) can occur. The same problems can also occur in the thoracic spine (T-spine) - although less common. Before we say how a herniated disc and a spinal gland are treated, we answer the question: What is the thoracic spine?
Well, the thoracic spine is the section between the cervical and lumbar spine. The thoracic spine is made of 12 vertebrae. It forms a unit with the ribs, the ribcage and the sternum. The thoracic spine has several tasks - the most important one is the protection of the spinal cord, located in the spinal canal. Unfortunately, back pain has become a common disease. About 80% have back pain at least once in their lives. Often, nonspecific back pain disappears on its own or after conservative treatment, but in case it lasts longer, becomes unbearable and radiates you should consult a specialist. He/she will be able to diagnose what's behind it: possibly a narrowing of the spinal canal, herniated disc or a tumor.
"To be, or not to be – that is the question" - Conservative methods or microsurgical surgery?
Often, back problems can be cured by conservative therapies but if they are not enough, a specific treatment must be carried out; in fact in case of herniated discs or spinal canal stenosis microsurgical measures must be used. The starting point of a correct diagnosis is the anamnesis, which means the conversation between doctor and patients in which the first one will ask his questions and the second one will answer. Where does it hurt? Since when? How acute is pain? Does it radiate? Answer honestly and as detailed as possible. After all, there is – although invisible - a connection between mind, body and soul. Visible answers are received through imaging techniques: MRI (magnetic resonance imaging) and/or CT (computed tomography). Of course, with spinal stenosis of the thoracic spine, it is important to know exactly where it is located.
Herniated discs in the thoracic spine are much rarer than, for example, in the lumbar spine, but they should not be underestimated. They cause usually acute pain. In fact, they can lead to paraplegia. The stenosis, which occurs preferably between the 50th and 80th years of life, has predominantly these symptoms which usually intensify slowly: Gait insecurity, numbness of the legs or loss of strength of the legs. You can walk only a few hundred meters, get tired, have heavy legs, every step can be an agony. It can lead to malfunction of the urinary and genital area, possibly even to incontinence – i. e. uncontrolled loss of urine. These symptoms usually develop slowly.
With a herniated disc in the thoracic spine, patients feel stinging pain in the affected part of the back. They are usually felt as a slight pain felt between the shoulder blades and pull themselves with a circular shape over the chest. Pain can be increased by sneezing or coughing. Patients that feel tightness in the chest can fell also tachycardia and heart stuttering, misinterpreting it with a heart attack. In case of tumors and cysts in the thoracic spine, patients complain of radiating pain into the legs, numbness, decreased strength and/or bladder dysfunction. The symptoms may develop slowly in benign tumors (meningiomas or neurinomas) or aggressively and relatively quickly in metastases.
What should you do? Herniated disc can be conservatively treated with physiotherapy and medication. The conservative therapy methods include heat therapy, electrotherapy and exercise therapy which will help the patient to relieve and stabilize the spine. Targeted strengthening training for the back and abdominal muscles and support corsets (orthoses) can also be helpful to relieve the spine. If conservative methods are not enough to relieve patients from pain caused by herniated discs and stenosis, we recommend minimally invasive surgical techniques that relieve squeezed nerve roots from prolapsed disc tissue or dilate narrowed spinal canals. The respective findings and your general health condition will allow us to talk about the therapy options you have and to choose the right one.
Operation procedure - microsurgical decompression is the method of choice
In contrast to conventional surgical procedures, a small incision (of about 3 centimeters) is sufficient in microsurgery for 1 level. The main advantage is that it significantly reduces the risk of subsequent scarring.
Under general anesthesia, we reach the affected vertebrae or intervertebral disc by inserting the probe directly. Once the affected area is reached we remove excess tissue and slightly dilate the area which will relieve the nerve root from any kind of pressure. If there is a cyst or tumor it will be removed. In case of syringomyelia, the cyst is opened. The main purpose of microsurgical procedures is always to relive the spinal cord from any kind of pressure. The so-called decompression (pressure relief) of constricted nerves is the most frequently selected treatment methods. During the treatment the doctor uses a microscope and/or an endoscope to have a greater visual radius and guarantee a precise treatment.
Immediately after the procedure
Slowly and under supervision, you will come back to the recovery room, where your health conditions will be monitored. After that, a nurse will accompany you to your room, where you will continue to be subjected to check ups and then begin to make the first movements. You will also be given medicines for example painkillers.
Post-operative days
The post-operative inpatient period is of about 8-12 days. Patients are not able to work for about 4-10 weeks. They need to slowly get used to life again - driving is possible after about 4 weeks, but initially only short distances can be traveled. To swim in a backstroke style is possible after four weeks and in a breaststroke style after four months. You cannot do jogging; golf or tennis - for at least 3-4 months. Cycling is likely to be possible in ten weeks.
Note: These are all just guidelines - your condition and your specialist will decide individually when and what is possible to do paying attention to not endanger the success of treatment.
Minimally invasive operations have been considered low-risk procedures for years
Of course: it is an operative procedure, and complications cannot be fully excluded. Complications are seldom and include bleeding, wound infection or swelling. Adhesions are not excluded in the area of the nerve root, which then again lead to pain and discomfort. But basically (and normally) you can assume that your pain belongs to the past. Against scarring, an anti-scar gel is injected around the neural structures.
Attention: Please respect the agreed check-up's appointments. And go immediately to the doctor if you get a high fever and severe pain or if you see redness and/or signs of inflammation at the wound. It is: Better once again by the doctor than once again late. In case you are unsure about any side effects, you can also ask for a medical opinion by phone.
The Avicenna Clinic in Berlin is always willing to help you
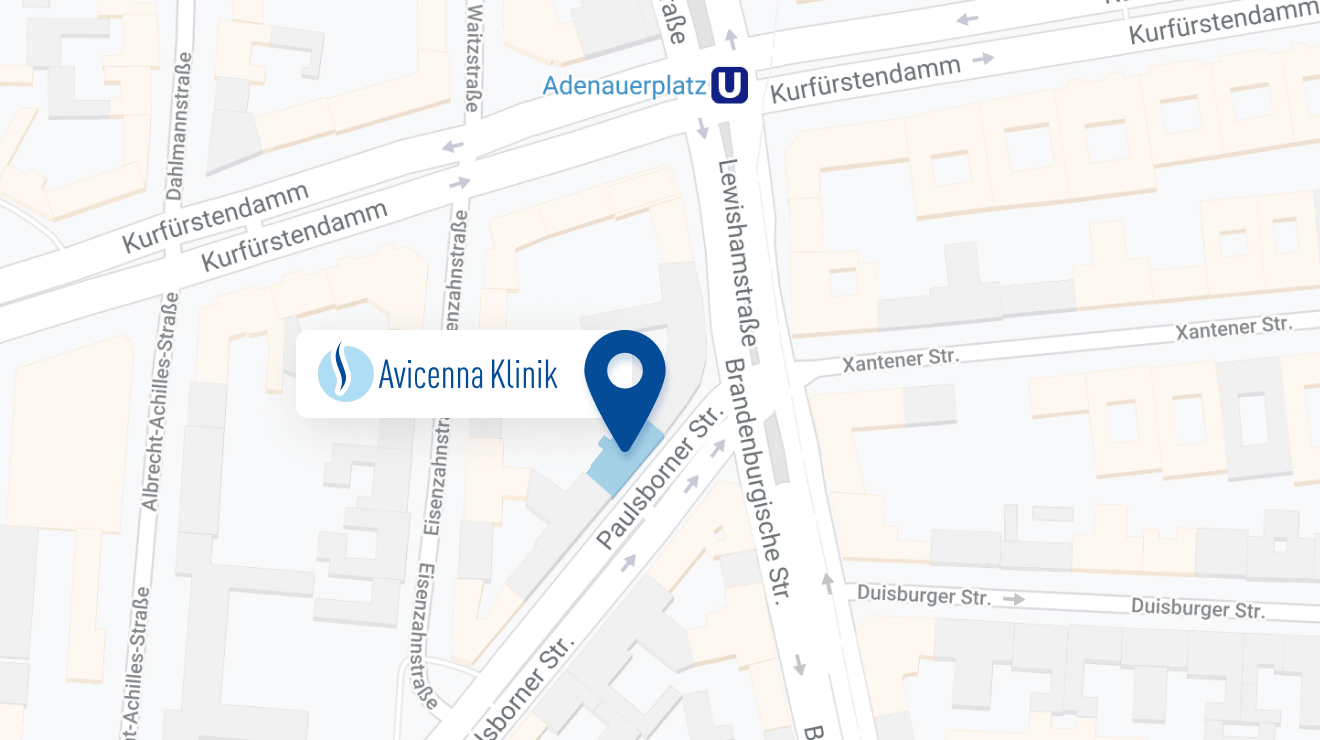
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: