What is a herniated disc in the cervical spine?
A herniated disc is a rupture of the gelatinous core of an intervertebral disc through the fibrous ring into the spinal canal. The leaked material presses on the spinal cord or spinal nerves (spinal cord nerves). Herniated disc in the cervical spine has a technical term: cervical disc hernia. Intervertebral discs, are the small shock absorbers between each vertebra. The intervertebral discs consist of a generally soft, gelatinous core and a firm outer fibrous ring whose lamellae provide the necessary stability.

What happens with a herniated disc of the cervical spine?
The intervertebral discs in the human body function much like shock absorbers: they take on a bumper function by absorbing shocks and impacts. In addition, we owe the mobility in our back to the intervertebral discs, because they enable the rotational movements of our spine. Our intervertebral discs are located between two vertebral bodies and consist of two components: The inner, soft gelatinous core and the surrounding fibrous ring.
Each vertebra has an arch-shaped section, the vertebral arch. Together, the vertebral arches form the spinal canal ( vertebral canal), along which the spinal cord passes. In each space between the vertebrae, spinal nerves branch off to the side.
In the case of a herniated disc, the soft gelatinous core emerges from the disc through the fibrous ring and then presses on the spinal cord or spinal nerves. We speak of a herniated disc of the cervical spine when the disc prolapses between the vertebrae C2 to TH1.
Smaller disc herniations are called prolapse, disc protrusion, in other words, protrusion. Larger or more extensive herniations, on the other hand, are called sequestra.
The consequences of a herniated disc in the cervical spine are pain, restricted mobility, and even paralysis. We will go into the exact symptoms later on.
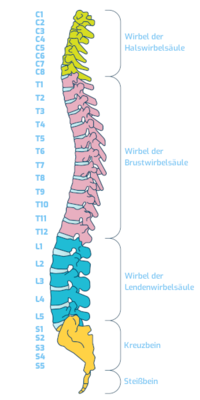
Structure of the cervical spine
The cervical spine consists of seven vertebrae, numbered C1 to C7. The C stands for cervix, Latin for neck or nape of the neck. The special thing about the structure of the cervical spine is that there are no intervertebral discs between the skull and the first cervical vertebra (atlas), or between the atlas and the 2nd cervical vertebra. This means that there are only 6 intervertebral discs in the cervical spine, if you include the last intervertebral disc between the 7th cervical vertebra and the 1st thoracic vertebra.
A herniated disc in the cervical spine usually affects the lower region, i.e. between the 5th and 6th cervical vertebrae and between the 6th and 7th vertebrae. The intervertebral discs between the cervical vertebrae C2 to C4 are rather rarely the trigger for a herniated disc.
Not infrequently, compression of the cervical spine is caused by ossifications (osteophytes), which additionally increase the narrowing of the spinal canal or the neuroforamen (nerve exit opening).
Causes of cervical spine disc herniation
It is unfortunately the truth: mainly older people are affected by a herniated disc in the cervical spine. The reason for this is that degenerative signs of wear and tear on the spine favor a herniated disc. The fibrous ring no longer has the stability and elasticity to withstand the pressure of the inner gelatinous core.
Wear and tear of the cervical spine is a gradual process. It begins as early as the age of 20 and the incidence of disease increases thereafter. Especially intensive is this abrasion of the spine and the fibrous rings up to the age of 45. Therefore, younger people may already suffer from limitations, discomfort and even herniated discs.
Of course, there are other determining factors for a herniated cervical spine disc besides degenerative causes. These include, for example, constant incorrect strain, tech neck (due to excessive or incorrect use of cell phones and PCs), car, sports or other accidents with high impact speeds. The risk of a herniated disc is increased by being overweight, lack of exercise, faulty posture and heavy lifting.
The symptoms of a herniated disc in the cervical spine
The specific symptoms of a herniated disc in the cervical spine depend on two factors:
- The level of the herniated disc in the cervical spine
- The question of whether the leaked material presses on the spinal cord or laterally on the spinal nerves
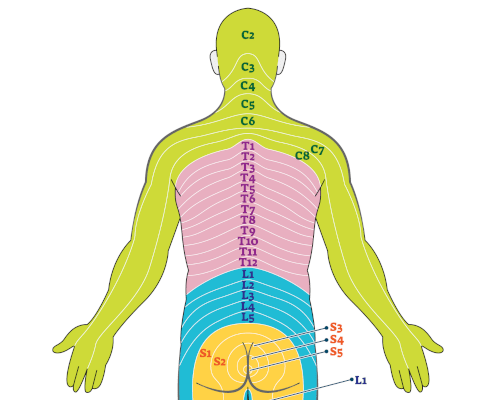
Based on the patient's complaints and symptoms, the positioning of the prolapse can already be identified. The reason for this is based on the fact that typical symptoms can be assigned to the individual segments of the cervical spine. In medical terms, this can be explained by the fact that the nerves branching off from the spinal cord send stimuli to specific areas of the shoulders, arms and fingers. These areas of the skin are called dermatomes.
Example: If a patient experiences numbness, pain, and motor limitations throughout the arm and into the thumb, the sixth spinal nerve is probably affected. If the seventh spinal nerve were restricted by the leaked material of the gelatinous nucleus, impairment and pain would be present in the index and middle fingers.
The symptoms of a herniated disc in the cervical spine are dependent to a large extent on the exact position of the vertebrae.
What symptoms do I experience with a herniated cervical disc?
A herniated disc in the cervical spine does not always manifest itself with pain symptoms. However, when nerve roots are irritated or put under pressure, neck pain is common. This pain can radiate to the shoulder blades as well as the arms. Additionally, numbness may begin in the arms and fingers. Headaches, difficulty concentrating, dizziness, tinnitus, disturbance of balance or visual disturbances also occasionally occur. Muscle weakness in the arms indicates a more serious disc herniation or severe narrowing of the spinal canal.
Patients may later develop other rare symptoms such as loss of control of the extremities, deterioration of handwriting, bladder emptying problems, difficulty breathing with lower oxygen saturation (especially when sleeping), stiffness or twitching of the arm and leg muscles, atrophy especially of the hand muscles, and therefore disturbances in fine motor skills.
Very important: if you experience one or even more of these symptoms, it is absolutely high time to see the specialist.
The symptoms at a glance
- Neck pain and stiffness, often with radiation of pain to the shoulders
- Pain, weakness, and disability in the head, shoulder, arm, hand, and even the fingers
- Sensory disturbances, paralysis and paralytic symptoms of the arms and hands
- Tingling or numbness in shoulder, arm or hand
- Rare: Difficulty concentrating, dizziness, tinnitus, disturbance of balance, or visual disturbances
Diagnosis? Tell your doctor where you feel pain
Before therapy for a herniated disc of the cervical spine may begin, an accurate diagnosis is most important. The definition for the word "diagnosis": it is the evaluative summary of a patient's symptoms and diagnostic findings, culminating in the identification and naming of the underlying disease.
Diagnosis begins with a conversation - history taking between the doctor and the patient. In a conversation like this, facts are gathered, such as:
- When did the pain start?
- Where did it start in the neck?
- Did it spread - to the hands?
- Did it change the walk?
- Are there any psychological problems?
- Where do you feel numbness?
- Do you feel tingling in your fingers?
- Where do you feel weakness?
After the interview, the specialist examines the limitations in flexibility and range of motion of the cervical spine but also reflexes (lively or weakened), pathological reflexes (Hoffmann and Trömner reflexes), sensitivity, strength, stiffness, atrophy, balance (Romberg's sign).
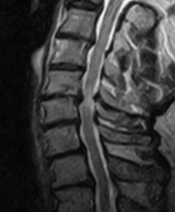
Then the doctor has an extensive diagnostic procedure at his disposal. The best view of the inside of the body is provided by technology: X-ray examination, computed tomography (CT) and especially magnetic resonance imaging (MRI). MRI primarily shows the localization and extent of disc wear in the cervical spine. It also shows the neural structures and adjacent segments in detail. The MRI shows whether nerve root, vertebral body or even spinal cord would be affected (exclusion of myelopathy).
Before surgery, conservative therapies can help
In Germany, 200,000 people undergo cervical spine surgery every year to reduce pressure on the spinal cord or on the nerve roots in the cervical spine.
Before we recommend surgery at the Avicenna Klinik , conservative therapies could possibly help, especially for pain and tension: Medication therapy, injections, computed tomography (CT)-guided injections (PRT), infusions, physical therapy, physiotherapy, manual therapy, osteopathy, electrotherapy and others.
In the Avicenna Clinic we offer several individual interventions. They are all discussed with the patient in detailed consultations and are basically based on the severity of the incident, the severity of the symptoms, the presence of neurological deficit and signs of spinal cord damage. Here, we treat the cause and not just the symptoms.
Minimally Invasive Percutaneous Laser Disc Decompression (PLDD)
One surgical option is minimally invasive percutaneous laser disc decompression (PLDD). PLDD is a particularly low-risk procedure. It does not require opening the spinal canal or damaging or removing surrounding tissue. Decompression of the intervertebral disc by laser is a procedure that has been tried and tested for decades and has been and is constantly being further developed. The first time this procedure has been used to relieve pain was in 1987.
What is this procedure all about? The goal of this treatment is to shrink the protrusion) of the disc and relieve the neural structures. The painful nerve fibers that have penetrated the disc due to degeneration are eliminated by laser. The method of percutaneous laser disc decompression (PLDD) achieves very good results, especially in the case of strong small disc protrusions and smaller herniated discs of the cervical spine. The pain is significantly relieved by the laser treatment of the nerves.
Minimally invasive percutaneous nucleotomy (PN)
Another option is the minimally invasive percutaneous nucleotomy (PN). A nucleotomy becomes necessary when nerves are pinched off or squeezed by the prolapsed portions of the disc. This method is a good option to use in the cervical spine (CS).
The minimally invasive procedure takes about 30 to 45 minutes, and it has the major advantages of not opening the spinal canal. So the point of percutaneous nucleotomy is not to remove the entire disc - rather, the goal is to remove disc tissue, thereby relieving and exposing the distressed nerve root.
Microsurgery on the cervical spine
If there is a significant herniated disc or a clear spinal canal stenosis of the cervical spine, microsurgery is recommended. This cervical spine surgery under general anesthesia is usually performed from the front (ventral) through a transverse skin incision about 5 centimeters long. The affected disc is removed with the aid of a special surgical microscope and micro-instruments. The herniation or ossifications are then removed until the neural structures are completely relieved. An anti-scar gel is administered in the surgical field.
As a replacement for the affected disc, a disc prosthesis or a cage is implanted, possibly with plating. The disc prosthesis (artificial disc, intervertebral disc prosthesis) allows good mobility of the segment and puts much less strain on the surrounding segments. Plating (cage with plate) or fusion (spondylodesis) provides stability.
Are you asking yourself whether a disc prosthesis or a cage is better? There are strict rules that determine whether a prosthesis or a cage/plate should be implanted. Other than the two options, a vertebral body replacement with additional plating is necessary for severe wear disorders with significant deformities or instabilities.
Patients with allergies to titanium, cobalt, chromium, or plastic (a component of several implants) benefit greatly from carbon implants, which also produce excellent results. We prevent late allergic reactions with carbon implants.
Rarely is the dorsal approach (from behind) necessary, and even more rarely is additional dorsal stabilization (screw fixation) necessary.
What is the right therapy for the herniated disc in the cervical spine?
Which of these therapy methods for the treatment of the herniated disc in the cervical spine is suitable in your case, what are the disadvantages and advantages for you: You will find out when you talk to our doctors during a detailed consultation and after the neurological examination and assessment of your MRI or CT images.
Prognosis for herniated disc of the cervical spine
The prognosis for a herniated disc of the cervical spine can be summarized in one short sentence: Everything will be fine again! The pain in the neck will disappear as well as the paralysis and paralytic symptoms. Soon you can expect the usual movement of the spine again and slowly return to appropriate exercises and loads.
The spoilsport of your good mood has been removed from your body by your neurosurgeon. Now the focus is back on the future. And that means: on the first day after your cervical spine surgery, you are already up and about. Of course, a nurse or caregiver will be with you the day after surgery, because your circulation is still quite weak. A neck brace will protect you from careless neck movements. It is absolutely essential that you have someone pick you up, as you are not allowed to drive yourself. Ideally, your place in the car for the next four weeks is not behind the steering wheel, but behind the glove compartment.
How long you are absent from work and receive sick leave? That depends on your profession! If you have to carry heavy loads, you will have to take a break for eight weeks until the bone wound is completely healed. If you have a desk job, your boss can look forward to seeing you in as little as 4 weeks. In other words: Your grace period depends on the recovery process and the physical demands of the job. Sports? Sure, but no soccer, no volleyball, no ski jumping, no golf, etc. Go for a walk, every walk is massage for your cervical spine and your soul. Consider rehabilitation to rethink nutrition and work habits.
One more thing: Be patient with yourself after cervical surgery. Don't take the necessary surgery on your cervical spine, the necessary time off that comes with it, as a debacle, but rather as a beckoning from fate to give you a rest that you would never have allowed yourself otherwise. In the future, take special care to heed back-friendly behavior. We recommend exercises to strengthen your back muscles. Visiting a back school or a physiotherapist will also help you reduce the risk of prolapse recurrence.
Frequently asked questions about the herniated disc of the cervical spine
Many questions arise about the diagnosis, symptoms and treatment of cervical disc herniations, which we are always happy to answer for our patients. We have listed the most frequently asked questions, including our answers, here.
What is not allowed? What to avoid?
It is important that you do not further overload your disc in the cervical spine. Therefore, in the case of a cervical spine disc herniation, avoid long car rides or a lot of time in front of the PC in particular. Often, patients unconsciously take exactly the position that caused the herniation.
In any case, you should also avoid types of movement that involve impact: jogging is a good example of this, as the intervertebral disc usually has to compensate for slight vibrations in the process. However, ball sports or sports that involve twisting the trunk (e.g. golf and tennis) are also not a good idea with a herniated disc of the cervical spine.
Herniated disc cervical spine - what to do?
If you suffer from typical disc herniation symptoms, there is one thing you can do first and foremost: seek out a doctor and have yourself examined. The specialist can evaluate the level of disc herniation and initiate appropriate therapies with you. Until then, avoid further stress.
Is a herniated disc in the cervical spine dangerous?
As a rule, a herniated disc in the cervical spine is accompanied by the typical symptoms that will limit you in your movements and everyday life. You may experience pain. However, a herniated cervical disc is only really dangerous if the leaked material presses not only on nerves but also on the spinal cord in the spinal canal. In this rather rare case, permanent nerve damage may occur, similar to spinal stenosis.
How long are you sick after a herniated disc of the cervical spine?
A precise statement on sick leave for a herniated disc in the cervical spine cannot be made in general terms and depends on many factors. How long you will be absent from work and receive sick leave depends greatly on your profession! If you have to carry heavy loads, you will have to take eight weeks off, until the bone wound is completely healed. If you have a desk job, your boss can look forward to seeing you in as little as four weeks. In other words: Your recovery period depends on the healing process and the physical demands of the job..
What helps with a herniated cervical disc?
In the case of a herniated disc of the cervical spine, conservative therapies often already help. This means that surgery can be avoided in many cases. Conservative forms of treatment include drug therapy, injections, computer tomography (CT)-guided injections (PRT), infusions, physiotherapy, physical therapy, manual therapy, osteopathy, electrotherapy.
Information about the article
The article was last checked and updated on September 9th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
Sources and further literature
W. Börm & F. Meyer. Spinale Neurochirurgie: Operatives Management von Wirbelsäulenerkrankungen. Schattauer. 1. Edition, Stuttgart 2008
M. Graf, C. Grill, H. Wedig. Beschleunigungsverletzung der Halswirbelsäule: HWS-Schleudertrauma. Steinkopff Verlag. Darmstadt 2009
A. König & U. Spetzger. Degenerative Diseases of the Cervical Spine: Therapeutic Management in the Subaxial Section. Springer Verlag. Luxemburg 2017
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: