What is vertebral slippage (spondylolisthesis)?
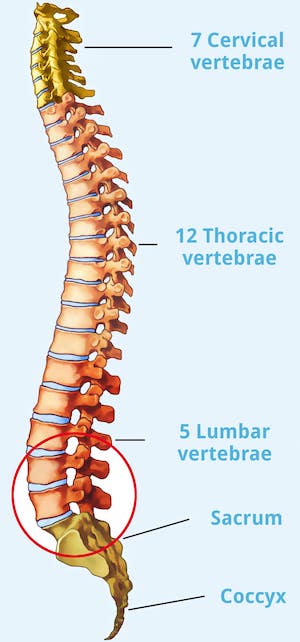
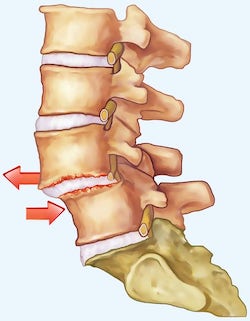
Vertebral slippage is a displacement of the vertebral body that leads to instability of the spine. This can cause a vertebra to slip forward (anterolisthesis) or backward (retrolisthesis) over the next lower vertebra. Vertebral slippage is also known as spondylolisthesis or simply listhesis. When a vertebra slips, its arch roots, transverse processes, and superior articular processes also shift.
Almost always, vertebral slippage affects the lumbar spine (LS). The 5th lumbar vertebra is the most commonly affected at 80 percent, and the 4th lumbar vertebra is the second most commonly affected at 15 percent. In addition, in most cases of a slipped vertebra there is a narrowing of the spinal canal, and rarely ganglion cystsganglion cysts. Due to the slow progression of the disease, more than half of all affected persons have unclear symptoms. Spondylolisthesis can be identified with the help of accurate diagnostics.
Symptoms of spondylolisthesis
The first signs of spondylolisthesis can be tingling and numbness in additional to back pain and leg pain. As a rule, pain on exertion and constant pain occur in the advanced stage. Preferably, this is severe pain after standing up or when turning around. During the day, the back pain usually increases. These complaints can cause nerve damage up to the functional loss of a nerve. This in turn can cause paralysis, which can affect the legs as well as the function of the bladder and bowels. At the same time, there may be more wear and tear on the intervertebral disc and vertebral joint. This can, apart from additional severe pain, also cause a herniated disc or spondylarthrosis. For this reason, spondylolisthesis must be treated as soon as it is diagnosed.
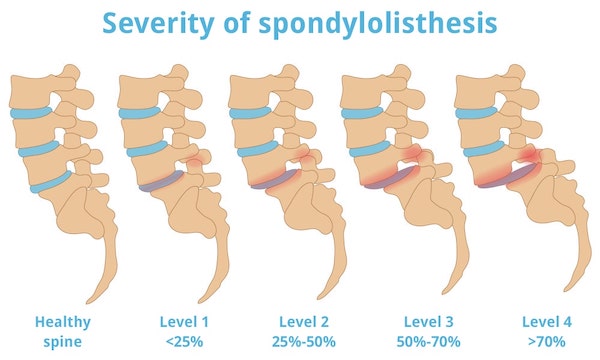
The severity of spondylolisthesis
In spondylolisthesis, the vertebrae are no longer positioned normally on top of each other. Viewed from the side, they are displaced against each other. Basically, four degrees of severity can be distinguished in vertebral slippage, which are determined by the orthopedist or a neurosurgeon. According to Meyerding's classification from 1932, the degree of slippage is given as a percentage of the vertebral body depth.
These are the degrees of severity of spondylolisthesis:
- Grade 1: less than 25% displaced. The upper vertebral body covers at least three-quarters of the covering plate of the lower vertebral body.
- Grade 2: 25 to 50 %. The upper vertebral body covers at least half but less than three-quarters of the covering plate of the lower vertebral body.
- Grade 3: 51 to 75%. The upper vertebral body covers at least one-quarter but less than one-half of the covering plate of the lower vertebral body.
- Grade 4: more than 75% displaced. The upper vertebral body covers less than a quarter of the top plate of the lower vertebral body.
If the two adjacent vertebral bodies are no longer in contact with each other at all, this corresponds to 100 percent vertebral slippage. In this case, we speak of spondyloptosis, which is also seen as grade 5 on the severity scale. The respective degree of severity of spondylolisthesis is provided by imaging procedures such as X-rays, CT or MRI diagnostics.
Good to know The development from grade 1 to grade 4 is gradual in spondylolisthesis. This process does not take weeks, rather months or even years. If the slipped vertebra does not press on a nerve or directly on an intervertebral disc, vertebral slippage even proceeds largely without pain or symptoms in the large majority of patients. Only in rare cases can a sudden worsening of the spondylolisthesis occur. Die Entwicklung von Grad 1 bis zu Grad 4.
Causes of vertebral slippage
Normally, the spine forms a smooth, slight S-curve to which all components conform. Stability is provided by a strong muscle-tendon system.
There are various causes of spondylolisthesis: On the one hand, congenital deformations of the spine can cause the vertebrae to slip out of their usual position. On the other hand, gradual changes such as wear and tear on vertebrae and joints (spondyloarthrosis), bone resorption or previous fractures also lead to slipped vertebrae.
Furthermore, weakened back muscles, especially in old age, can cause spondylolisthesis. People between the ages of 50 and 60 are often affected. Over the years, the intervertebral discs, which act as shock absorbers between the individual vertebrae, lose fluid and thus volume. They become increasingly compressed and stand correspondingly closer together, loosening ligaments and tendons. The segments of the spinal column thus become unstable. The individual vertebra is no longer held in place and can slip out of its existing position more easily. Well-developed ligaments, muscles and tendons slow down the displacement because they provide additional support in the spinal canal.
In a few cases, listhesis can also be triggered by overuse of the spine in competitive sports. Artistic gymnasts, pole vaulters or dolphin swimmers are particularly at risk. Serious injuries, caused for example by traffic accidents, can also severely impair the stability of the spine and result in spondylolisthesis.
Typical causes of spondylolisthesis
Diagnosis of vertebral slippage
Since spondylolisthesis is a gradual process, patients often come to us with a different suspicion. Only with the help of a precise examination can the diagnosis of spondylosis be established.
The exact diagnosis therefore includes a whole package of measures to be able to distinguish slipped vertebra from other diseases. First of all, a detailed patient interview, an anamnesis, is necessary. Here, the doctor asks in particular about family strains or certain types of sport. He checks sensitivity, motor skills and reflexes to rule out damage to the nerves. This is followed by neurological-orthopedic examinations.
Among other things, an X-Ray of the back can be used to show vertebral displacements. X-rays in a flexed and extended position (flexion and anti-flexion) are necessary to confirm the diagnosis. Magnetic resonance therapy (MRI)is also helpful, as this technique can be used to show nerve roots, intervertebral discs, tendons and ligaments in detail.
Therapies for spondylolisthesis - this is how your specialist will help you
In some cases, treatment with conservative therapeutic therapies is sufficient to relieve the symptoms. As long as there are no neurological deficits such as paralysis, we always favor conservative treatment. In addition to treating the pain, we aim to stabilize the spine. As part of physiotherapy and back training, we strengthen the muscles in the back, or the patient is temporarily given a corset to keep the back in the correct shape.
If the discomfort and pain persist for a longer period of time, or if there are already deficits, we achieve good results in certain cases with a microsurgical operation. This improvement occurs by freeing the pinched nerves (decompression) and removing the narrowing and constriction. With subsequent strengthening of the back muscles, "natural" stabilization is achieved. In severe cases, spondylodesis (locking or stiffening) may be necessary in addition to decompression. With spondylodesis for spondylolisthesis, we free the pinched nerves (decompression), eliminate narrowing (stenosis), correct the position of the slipped vertebra (reduction) and stiffen the segment.
Spinal blocking is created by inserting elements made of titanium to stabilize loosened motion segments. During surgery, screws are inserted into the vertebral bodies for this purpose and fixed with connecting elements. The use of the body's own bone material provides more stability. A few months after the operation, the vertebral joints fuse with the inserted blocks or chips. In this way, the affected section is successfully stiffened. Rarely, a disc replacement is necessary. For patients allergic to titanium, implants made of carbon are used.
Glossary
Ventrolisthesis and anterolisthesis:
When a segment of the spine shifts forward relative to the underlying segment, we speak of ventrolisthesis. Another term for this process is anterolisthesis. Retrolisthese / Retrolisthesis:
Retrolisthesis is when the vertebral body slides backward compared to the underlying segment of the spine. Olisthesis and pseudolisthesis:
The term olisthesis is a shortened name for spondylolisthesis, i.e. vertebral slippage. Pseudolisthesis is the term used when vertebral slippage is caused by wear and tear. In some cases, pseudolisthesis is also called pseudospondylolisthesis.
What is spondylolisthesis?
Spondylolisthesis is a spinal disorder in which a vertebra is displaced toward an adjacent vertebra, putting pressure on the nerves in the spinal cord and surrounding structures. It can lead to a variety of symptoms, including pain, numbness, loss of strength and tingling.
What are the symptoms of spondylolisthesis?
The most common symptoms of spondylolisthesis are lower back pain, numbness in the legs, weakness and tingling. In more severe cases, it can cause irregular or severe pain in the lower back and legs.
Can spondylolisthesis occur to children?
Yes, spondylolisthesis can occur to children, although it is much more common to adults. While adults are often triggered by wear and tear, children are often triggered by trauma or a congenital malformation.
What are the different types of spondylolisthesis?
There are four types or degrees of severity of spondylolisthesis: These include Grade I (minor displacement), Grade II (moderate displacement), Grade III (severe displacement) and Grade IV (most severe displacement).
What treatments are used for spondylolisthesis?
There are several treatment options for spondylolisthesis, including conservative therapies such as physical therapy and medications, as well as surgical treatments. The type of treatment depends on the severity of the case and the symptoms.
information about the article
The article was last checked and updated on 16.02.2023.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: