What is a vertebral fracture?
The axis of the human body is the spine: it performs important static tasks and serves to protect internal organs and the spinal cord. The spine allows movement. For healthy people, the spine has a high degree of stability and it takes a lot of force to cause a vertebral fracture. The spine consists a total of seven cervical vertebrae, twelve thoracic vertebrae, five lumbar vertebrae, five fused sacral vertebrae and four to five tailbone vertebrae. Together with a complex ligamentous and muscular apparatus, the spine is therefore a functional, elastic system that can absorb loads.
You may have come to know a vertebral fracture by another name. There are these synonyms for spinal fracture: Vertebral Body Fracture, Fracture of the Vertebral Body, Compression Fracture, Impacted Fracture, Bending Fracture, Burst Fracture, Vertebral Body Fracture.
What causes a vertebral fracture?
A vertebral fracture of the actually very stable vertebral bones can occur if they are massively traumatized from the outside. These include traffic accidents such as car, bicycle and motorcycle crashes. Often named is also the head jump into shallow water, more often occur falls, sports and violence as a cause. A vertebral body fracture only happens in case of a large external force impact. The muscles cannot absorb an impact of extreme dimensions. In addition, the spine is slowed down on one side during the fall. The vertebral body strikes and breaks. This results in a vertebral fracture (fractura vertebrae). Bone loss (osteoporosis) can lead to vertebral fractures, even without serious external effects.
A vertebral fracture can affect the spinous process, the vertebral body or the vertebral arch. A complication that is most feared by those affected is paraplegia, a life in a wheelchair. Many know the fate of Samuel Koch, who had an accident during a "Wetten dass...?" show and has been in a wheelchair with spinal cord injuries ever since. A spectacular performance turned into a drama: Koch broke his neck four times during an unsuccessful jump over a moving car. The sad result is permanent paralysis.
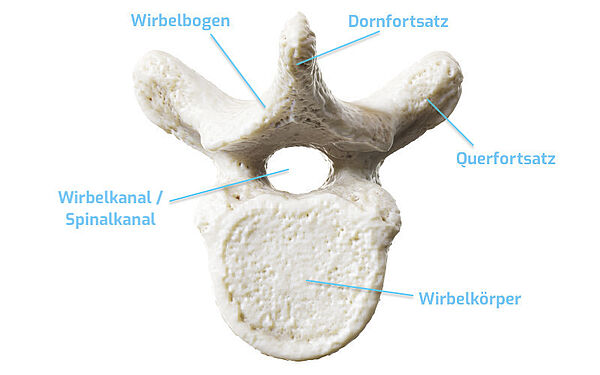
The structure of the human vertebra
Before we discuss the vertebral fracture and further explain how such a fracture can occur and how it should be treated, we would first explain the vertebra. What does it look like? What is its structure?
The vertebrae in the cervical spine, thoracic spine and lumbar spine have similarities, but there are also differences.
Let's start with the parallels in the structure of the vertebrae: They all have the same bony structure and consist of:
- the vertebral body - lat. corpus vertebrae, it is the actual load-bearing and supporting part of the spine. The inner part is filled with red bone marrow, the upper and lower parts are porous.
- the vertebral arch
- two transverse processes
- one spinous process
- four articular processes, two upper and two lower articular connections to the neighboring vertebrae.
Differences between vertebrae of the cervical spine, thoracic spine and lumbar spine
As is well known, the spinal column has different functions and burdens in its individual spinal segments. The vertebrae in the lumbar spine basically have to bear the greater weight and are accordingly more strongly equipped compared to the cervical vertebrae. They must allow for a high degree of mobility, but unlike the lumbar spine, it is not their job to support large weights. The so-called atlas, which supports the head, is the first cervical vertebra. It does not have a vertebral body, but is connected to the second vertebral body by a joint.
In the vertebral canal, formed by the vertebral holes of single vertebrae, runs the spinal cord, which together with the brain forms the central nervous system. The vertebral canal (canalis vertebralis) is also called the spinal canal or spinal cord canal.
Vertebral fractures - the lumbar spine is most frequently affected
Around 250,000 vertebral hernias (vertebral fractures), which also include vertebral body fractures, occur in Germany every year. While traffic and sports accidents are usually the causes of vertebral fractures in younger people, vertebral fractures in older people are mainly due to a weak bone structure caused by osteoporosis. In 20% of accidental fractures, two or more vertebrae are affected. One in two patients (54.4%) sustains a collateral injury. And the risk of suffering a neurological deficit increases significantly with increasing injury intensity, so that about 53 percent of patients even suffer from myelopathy. Vertebral fractures are most commonly seen in the lumbar spine (LS) or thoracic spine (TCS).
Causes of vertebral fracture - from accident to osteoporosis
The words 'accident' and carelessness' keep coming up when we talk about the causes of traumatic vertebral fractures. Someone has fallen down the stairs or off the ladder. Someone took a punch, or someone took a dive into the water, not knowing that the water was shallow. Someone did an unfortunate tumble on the gymnastics mat in gym class, or slipped on wet leaves in icy conditions or in the fall. Violence can also be a cause. There are hundreds of ways to fracture a vertebra in an accident (self-inflicted or not). The areas between the cervical spine and thoracic spine, between the thoracic spine and lumbar spine, and between the lumbar spine and the sacrum are considered particularly vulnerable to injury.
Osteoporosis - the great danger for a vertebral fracture
In addition to traumatic fractures, so-called pathological fractures also occur very often, such as in osteoporosis. It is also called "bone atrophy". Osteoporosis is a chronic, slow disease of the bones, which often begins in earlier adulthood. Osteoporosis can cause osteoporotic fractures, primarily of the hip and spine, without significant external influence. In fact, sometimes harmless occasions, such as a sudden coughing attack or carrying a shopping bag, are enough for a spontaneous fracture to occur. Osteoporosis is the most common cause of a fracture of a vertebral body. The cylinder-shaped vertebral bodies form the basic framework of the spinal column.
Why are osteoporosis patients so particularly at risk of suffering a fracture that can cause severe pain? Well, osteoporosis is a metabolic skeletal disease. As a result, there is a reduction of bone mass. Osteoporosis patients suffer from what is known as bone density: it refers to the relation of mineralized bone mass to bone volume. The actual balance between bone formation and degradation is shifted. The result: porous, increasingly thin bones that can break easily. Bone loss!
The most common location for an osteoporosis fracture is the 7th thoracic vertebra or between the 11th thoracic vertebra and the first lumbar vertebra. Tragically, many osteoporosis patients suffer not just one fracture in their lifetime, but three, four, even five fractures. And it's not always just the spine that is affected: the thighs, lower and upper arms, pelvis, sacrum, ribs and sternum are also at risk. Interestingly, it is not only older people who suffer from osteoporosis; many younger people are also affected by bone loss. Osteoporosis patients belong in the hands of a specialist, an osteologist. He or she treats people with insufficient bone substance.
Other causes of vertebral fractures
Bone cancer or metastases to the skeleton, spondylitis (bone inflammation), bone softening (osteomalacia) and rheumatism are also possible triggers for a vertebral fracture. In these cases, the vertebral fracture sets in without any visible injury.
Vertebral fracture - these are the symptoms
The symptoms of a vertebral fracture: Depending on the location of the fracture, there is pain over the injured vertebral body and the neighboring spinal segments. Major injuries are always accompanied by considerable pain symptoms. If, for example, the vertebral fracture traps the spinal cord, motor function failures or impaired sensitivity may occur.
Frequently patients experience sudden back pain when they injure the spine - often with pronounced movement restrictions and the appearance of mild paralysis. Depending on the structures affected, sensory disturbances such as tingling or numbness also occur. These can radiate to the arms and legs. Symptoms of a whiplash injury of the cervical spine (HWS) occur in some cases even after a few days.
Patients often do not see a doctor until a vertebral fracture presses on surrounding structures and causes pain. This is when symptoms such as paralysis in the limbs or disturbances in sensitivity become obvious.
Important: Do not hesitate to call an ambulance if any of the above symptoms occur. A spinal fracture is a serious injury that must be treated by a specialist as soon as possible.
Diagnosis vertebral fracture - this is how a doctor can identify the fracture
Diagnostics includes the preliminary consultation between the doctor and the patient - the so-called anamnesis conversation. We say this explicitly because you must please internalize that this conversation is important. Therefore, make sure that the doctor takes time for you, that he listens to you. And take your time, too! Tell the specialist if there has been a fall, accident, exposure to violence or other potentially triggering event.
Tell the doctor if you have already experienced paralysis, numbness in your arms or legs, or problems with uncontrolled urination or bowel movements. Also tell him if you have trouble swallowing. He will also ask you about any pre-existing conditions related to the skeletal system - answer clearly and in such a helpful way as to allow the doctor to make a truly accurate diagnosis. Because only an accurate diagnosis gives him the opportunity to successfully treat, to help you.
The anamnesis is followed by a detailed physical and neurological examination. After the doctor has made a tentative diagnosis of vertebral fracture based on his examination, he orders diagnostic imaging procedures.
With the help of an X-Ray, computer tomography (CT) and/or MRI (magnetic resonance tomography), the doctor can view the vertebral fracture and also clearly see what type of fracture and what extent it actually is. On this basis, the doctor and patient decide about the further treatment of the vertebral fracture. Further examinations such as bone density measurement or neurophysiological examinations are often necessary.
During the clinical examination, the doctor checks whether walking or standing is possible, a check of mobility in other words. To see if there are any neurological deficits, cranial nerves, sensitivity and motor function are checked.
Stable or unstable vertebral fracture?
For the diagnosis of the vertebral fracture you should still know: Basically, the doctor diagnoses either a stable or an unstable vertebral fracture. In stable fractures, soft tissues and ligaments are not affected, and the spinal canal is not narrowed. Fortunately, about 85 percent of all spinal fractures are stable fractures. They usually heal without surgery. An unstable vertebral fracture occurs when the affected spinal segment has been deformed by forces acting from different directions. These include, for example, distraction injuries (type B) and rotational injuries (type C). An unstable vertebral fracture can lead to paraplegia.
Classification for the assessment of vertebral fractures
In 1994, Friedrich Paul Magerl (*May 21, 1931 in Styria, Austria), an Austrian surgeon and pioneer of spine surgery, introduced a classification for the evaluation of thoracic and lumbar spine injuries that is still commonly used for assessment today.
- Typ A: Compression injuries: In this case, the vertebra is compressed. This happens mainly in the front region of the vertebrae.
- Typ B: Distraction injuries: A torque causes the vertebra to break in the transverse direction. Such injuries occur predominantly in the back of the vertebra.
- Typ C: Rotational injuries: They occur during turning. Longitudinal ligaments and not unusual intervertebral discs are also affected.
Fracture of the lumbar spine - can it be treated successfully?
The successful treatment of a vertebral fracture depends on many factors. The treatment of a vertebral fracture varies from immobilization and physiotherapy to interventions such as stabilization, vertebral body replacement or kyphoplasty, including cage (placeholder) implantation. Kyphoplasty is a minimally invasive percutaneous procedure that rebuilds fractured or fragile vertebrae using bone cement.
Depending on the severity of the fracture to one or more vertebral bodies, the treatment and procedures to be used are decided. Mild sprains of vertebral bodies, soft tissue injuries and smooth, stable fractures usually do not require surgery. We achieve a good chance of recovery with conservative therapies, which, depending on the injury, include pain management, orthoses (supportive corsets, i.e. immobilization), massage, electrotherapy, physiotherapy, heat or cold applications or pain psychotherapy, or simply rest.
In some cases, vertebral body replacement or a combination of the above procedures is necessary. The most suitable method in each individual case depends on the type of injury (including how stable or unstable the fracture is, where the fracture site is located, how the fracture lines run, how deep bone fragments are in the spinal canal) and also on the patient's age.
In the case of a complicated vertebral fracture with displaced fracture edges or splinters, we have various operations at our disposal. With the help of microsurgery we relieve the neural (nerve) structures. In some cases stabilization measures (spondylodesis) are necessary. In this case, we perform a blocking (stiffening, fusion, plating) of the affected spinal segment. Other therapy optionsmay also be considered here.
The goal of surgical treatment is to quickly realign and stabilize the spine in order to relieve pressure on the nerves as quickly as possible. The stability of the vertebral bodies and therefore the spine must be restored in order to be able to relieve the pain and protect the spinal cord.
Prognosis - how are the long-term effects?
Unfortunately, there are no clear rules when it comes to prognosis after a vertebral fracture. And it would also be irresponsible if we did not state this so clearly. A bit of luck and - of course - a back-friendly behavior are part of it, in order to live with little or no pain after the treatment. Basically we can say: The healing time for a vertebral fracture depends on how serious the injuries are. A stable vertebral fracture will usually become bone solid again after a few weeks or months without shifting further. You will therefore get back on your feet relatively quickly and will ideally be able to live without consequential damage and late effects.
Vertebral fractures and pregnancy
Dr. Munther Sabarini: " Repeatedly, I am asked by women who need surgery after a fall or other accident, 'Doctor can I still have a baby after this?' I can understand this anxious question very well. But I can also reassure. Surgery after a stable vertebral fracture - unless there are other reasons - will not prevent pregnancy. I know many women who had a happy pregnancy and gave birth to healthy babies despite the surgery.
Healing time for unstable vertebral fractures varies
Of course, you have to know: The healing period after unstable vertebral fractures can last up to half a year or even longer. Unfortunately, it must be said that despite a good healing process, pain and reduced mobility may remain. The length of time for healing of a vertebral fracture varies greatly in each case. Many factors such as age, extent of the injury and also the subsequent treatment influence the recovery.
That's why it's even more important to take care of yourself! If you practice high-risk sports, you should always wear the right protective clothing. After all, it's no secret that motorcycling, snowboarding and show jumping, for example, pose a high risk of suffering a fractured vertebrae. Motorcyclists should never start the machine without the proper protective gear if they don't want to risk fracturing their vertebrae. In high-risk sports, putting on so-called back protectors can often prevent bad things from happening.
Information about the article
The article was last checked and updated on August 23th, 2022.
About the author
Dr. med. Munther Sabarini, MD, is the director and founder of the Avicenna Clinic. As a specialist neurosurgeon, he particularly has expertise in the treatment of spinal disorders. Dr. Munther Sabarini has more than 30 years of professional experience. During this time he treated more than 30,000 patients.
Avicenna Clinic Content Quality Guidelines
All texts and content are written by medically trained, experienced experts in the field. Learn more about our content quality guidelines.
Sources and further literature
S. Zwingenberger, A. Thomas, K.-D. Schauer, Alexander C. Disch. Klassifikation und Therapieempfehlung der osteoporotischen Wirbelkörperfraktur. Georg Thieme Verlag. 4. Ausgabe, Stuttgart, 2019.
Dietrich Grönemeyer. Mikrotherapie - Wirbelsäule. Georg Thieme Verlag. 1. Auflage, Stuttgart, 2022.
H. Reichel, H. Wipp, W. Hein. Wirbelsäulenchirurgie: Standortbestimmung und Trends. Steintopf Verlag. 1. Auflage, Darmstadt, 2000
A. Verheyden, U. Spiegl, A. Hölzl. DGU-Leitlinie: Verletzungen der thorakolumbalen Wirbelsäule. Deutsche Gesellschaft für Unfallchirurgie e.V. (DGU), Berlin, 2018.
The Avicenna Clinic in Berlin is always willing to help you
Since the year 2001, the Avicenna Clinic is based in Berlin. Our doctors have at least 25 years of international experience in their respective fields (neurosurgery, spinal surgery, anesthesia, and orthopedics).
If you have severe back pain, a herniated disc or a suspected herniation, please contact us using the following information: